by admin | May 1, 2018 | Benefit Management, Group Benefit Plans, HSA/HRA, IRS

Friday, April 27, the Internal Revenue Service (IRS) announced that the 2018 annual contribution limit to Health Savings Accounts (HSAs) for persons with family coverage under a qualifying High Deductible Health Plan (HDHP) is restored to $6,900. The single-coverage limit of $3,450 is not affected.
This is the final word on what has been an unusual back-and-forth saga. The 2018 family limit of $6,900 had been announced in May 2017. Following passage of the Tax Cuts and Jobs Act in December 2017, however, the IRS was required to modify the methodology used in determining annual inflation-adjusted benefit limits. On March 5, 2018, the IRS announced the 2018 family limit was reduced by $50, retroactively, from $6,900 to $6,850. Since the 2018 tax year was already in progress, this small change was going to require HSA trustees and recordkeepers to implement not-so-small fixes to their systems. The IRS has listened to appeals from the industry, and now is providing relief by reinstating the original 2018 family limit of $6,900.
Employers that offer HSAs to their workers will receive information from their HSA administrator or trustee regarding any updates needed in their payroll files, systems, and employee communications. Note that some administrators had held off making changes after the IRS announcement in March, with the hopes that the IRS would change its position and restore the original limit. So employers will need to consider their specific case with their administrator to determine what steps are needed now.
HSA Summary
An HSA is a tax-exempt savings account employees can use to pay for qualified health expenses. To be eligible to contribute to an HSA, an employee:
- Must be covered by a qualified high deductible health plan (HDHP);
- Must not have any disqualifying health coverage (called “impermissible non-HDHP coverage”);
- Must not be enrolled in Medicare; and
- May not be claimed as a dependent on someone else’s tax return.
HSA 2018 Limits
Limits apply to HSAs based on whether an individual has self-only or family coverage under the qualifying HDHP.
2018 HSA contribution limit:
- Single: $3,450
- Family: $6,900
- Catch-up contributions for those age 55 and older remains at $1,000
2018 HDHP minimum deductible (not applicable to preventive services):
- Single: $1,350
- Family: $2,700
2018 HDHP maximum out-of-pocket limit:
- Single: $6,650
- Family: $13,300*
*If the HDHP is a nongrandfathered plan, a per-person limit of $7,350 also will apply due to the ACA’s cost-sharing provision for essential health benefits.
Originally posted on thinkHR.com

by admin | Aug 29, 2017 | ACA, Health Plan Benchmarking
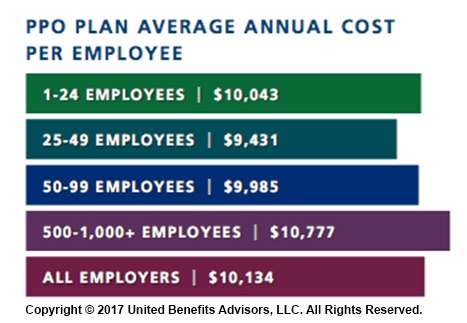
 Small employers, those with fewer than 100 employees, have a reputation for not offering health insurance benefits that are competitive with larger employers, but new survey data from UBA’s Health Plan Survey reveals they are keeping pace with the average employer and, in fact, doing a better job of containing costs.
Small employers, those with fewer than 100 employees, have a reputation for not offering health insurance benefits that are competitive with larger employers, but new survey data from UBA’s Health Plan Survey reveals they are keeping pace with the average employer and, in fact, doing a better job of containing costs.
According to our new special report: “Small Businesses Keeping Pace with Nationwide Health Trends,” employees across all plan types pay an average of $3,378 toward annual health insurance benefits, with their employer picking up the rest of the total cost of $9,727. Among small groups, employees pay $3,557, with their employer picking up the balance of $9,474 – only a 5.3 percent difference.
When looking at total average annual cost per employees for PPO plans, small businesses actually cut a better deal even compared to their largest counterparts—their costs are generally below average—and the same holds true for small businesses offering HMO and CDHP plans. (Keep in mind that relief such as grandmothering and the PACE Act helped many of these small groups stay in pre-ACA plans at better rates, unlike their larger counterparts.)
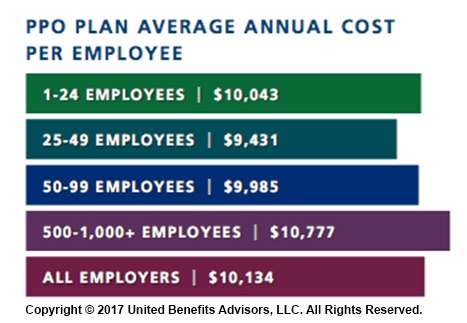
Think small businesses are cutting coverage to drive these bargains? Compared to the nations very largest groups, that may be true, but compared to average employers, small groups are highly competitive.
By Bill Olson
Originally Published By United Benefit Advisors

by Johnson and Dugan | Aug 2, 2017 | Benefit Management

Tired of celebrating the 10% increase? Join us in an innovative discussion on reducing your Health Insurance Premium through Creative Financing for your benefit program. Learn about turning a 10% increase into a 25% decrease.
Keynote Speaker:
Clifford Der, East West Administrators
We will be discussing alternative funding from traditional Self-Funding to Medical Expense Reimbursement Plans. We will also address any legal questions you may have regarding your liability as an employer offering a fully insured program versus a self-funded program.
11:45 a.m. – 12:00 p.m. Registration
12:00 p.m. – 1:00 p.m. Seminar & Complimentary Buffet Lunch
Location: Mistral Restaurant and Bar | 370-6 Bridge Parkway | Redwood Shores, CA 94065
Click Here To Register
About the Presenter:
Clifford Der, East West Administrators – Clifford has been a member of the National Association of Health Underwriters for more than 40 years. His extensive background in healthcare benefits includes developing the Chinese Community Health Plan (EPO-a first in the country), the first acupuncture plan, the development of the Medical Expenses Reimbursement Plans along with custom designed Partial Self-funded Health Plans.
Sponsored by:




by admin | Apr 28, 2017 | ACA, Benefit Management, Compliance
 While the health care affordability crisis has become so significant, questions still linger—will private exchanges become a viable solution for employers and payers, and will they will continue to grow? Back in 2015, Accenture estimated that 40 million people would be enrolled in private exchange programs by 2018; the way we see this model’s growth today doesn’t speak to that. So, what is preventing them from taking off as they were initially predicted? We rounded up a few reasons why the private exchange model’s growth may be delayed, or coming to a halt.
While the health care affordability crisis has become so significant, questions still linger—will private exchanges become a viable solution for employers and payers, and will they will continue to grow? Back in 2015, Accenture estimated that 40 million people would be enrolled in private exchange programs by 2018; the way we see this model’s growth today doesn’t speak to that. So, what is preventing them from taking off as they were initially predicted? We rounded up a few reasons why the private exchange model’s growth may be delayed, or coming to a halt.
They Are Not Easy to Deploy
There is a reason why customized benefits technology was the talk of the town over the last two years; it takes very little work up-front to customize your onboarding process. Alternatively, private exchange programs don’t hold the same reputation. The online platform selection, build, and test alone can get you three to six months into the weeds. Underwriting, which includes an analysis of the population’s demographics, family content, claims history, industry, and geographic location, will need to take place before obtaining plan pricing if you are a company of a certain size. Moreover, employee education can make up a significant time cost, as a lack of understanding and too many options can lead to an inevitable resistance to changing health plans. Using a broker, or an advisor, for this transition will prove a valuable asset should you choose to go this route.
A Lack of Education and a Relative Unfamiliarity Revolves Around Private Exchanges
Employers would rather spend their time running their businesses than understanding the distinctions between defined contribution and defined benefits models, let alone the true value proposition of private exchanges. With the ever-changing political landscape, employers are met with an additional challenge and are understandably concerned about the tax and legal implications of making these potential changes. They also worry that, because private exchanges are so new, they haven’t undergone proper testing to determine their ability to succeed, and early adoption of this model has yet to secure a favorable cost-benefit analysis that would encourage employers to convert to this new program.
They May Not Be Addressing All Key Employer and Payer Concerns
We see four key concerns stemming from employers and payers:
- Maintaining competitive benefits: Exceptional benefits have become a popular way for employers to differentiate themselves in recruiting and retaining top talent. What’s the irony? More options to choose from across providers and plans means employees lose access to group rates and can ultimately pay more, making certain benefits less. As millennials make up more of today’s workforce and continue to redefine the value they put behind benefits, many employers fear they’ll lose their competitive advantage with private exchanges when looking to recruit and retain new team members.
- Inexperienced private exchange administrators: Because many organizations have limited experience with private exchanges, they need an expert who can provide expertise and customer support for both them and their employees. Some administrators may not be up to snuff with what their employees need and expect.
- Margin compression: In the eyes of informed payers, multi-carrier exchanges not only commoditize health coverage, but perpetuate a concern that they could lead to higher fees. Furthermore, payers may have to go as far as pitching in for an individual brokerage commission on what was formerly a group sale.
- Disintermediation: Private exchanges essentially remove payer influence over employers. Bargaining power shifts from payers to employers and transfers a majority of the financial burden from these decisions back onto the payer.
It Potentially Serves as Only a Temporary Solution to Rising Health Care Costs
Although private exchanges help employers limit what they pay for health benefits, they have yet to be linked to controlling health care costs. Some experts argue that the increased bargaining power of employers forces insurers to be more competitive with their pricing, but there is a reduced incentive for employers to ask for those lower prices when providing multiple plans to payers. Instead, payers are left with the decision to educate themselves on the value of each plan. With premiums for family coverage continuing to rise year-over-year—faster than inflation, according to Forbes back in 2015—it seems private exchanges may only be a band-aid to an increasingly worrisome health care landscape.
Thus, at the end of it all, change is hard. Shifting payers’, employers’, and ultimately the market’s perspective on the projected long-term success of private exchanges will be difficult. But, if the market is essentially rejecting the model, shouldn’t we be paying attention?
By Paul Rooney, Originally Published By United Benefit Advisors

by admin | Apr 12, 2017 | Benefit Management, Employee Benefits, Human Resources
 With all of the focus that is put into managing and controlling health care costs today, it amazes me how many organizations still look past one of the most effective and least disruptive cost-saving strategies available to employers with 150 or more covered employees – self-funding your dental plan. There is a reason why dental insurers are not quick to suggest making a switch to a self-funded arrangement … it is called profit!
With all of the focus that is put into managing and controlling health care costs today, it amazes me how many organizations still look past one of the most effective and least disruptive cost-saving strategies available to employers with 150 or more covered employees – self-funding your dental plan. There is a reason why dental insurers are not quick to suggest making a switch to a self-funded arrangement … it is called profit!
Why self-fund dental?
We know that the notion of self-funding still makes some employers nervous. Don’t be nervous; here are the fundamental reasons why this requires little risk:
- When self-funding dental, your exposure as an employer is limited on any one plan member. Benefit maximums are typically between $1,000 and $2,000 per year.
- Dental claims are what we refer to as high frequency, low severity (meaning many claims, lower dollars per claim), which means that they are far less volatile and much more predictable from year to year.
- You pay for only what you use, an administrative fee paid to the third-party administrator (TPA) and the actual claims that are paid in any given month. That’s it!
Where do you save when you self-fund your dental?
Trend: In our ongoing analysis over the years, dental claims do not trend at anywhere near the rate that the actuaries from any given insurance company project (keep in mind these are very bright people that are paid to make sure that insurance companies are profitable). Therefore, insured rates are typically overstated.
Claims margin: This is money that insurance companies set aside for “claims fluctuation” (i.e., profit). For example, ABC Insurer (we’ll keep this anonymous) does not use paid claims in your renewal projection. They use incurred claims that are always somewhere between three and six percent higher than your actual paid claims. They then apply “trend,” a risk charge and retention to the overstated figures. This factor alone will result in insured rates that are overstated by five to eight percent on insured plans with ABC Insurer, when compared to self-funded ABC Insurer plans.
Risk charges: You do not pay them when you self-fund! This component of an insured rate can be anywhere from three to six percent of the premium.
Reserves: Money that an insurer sets aside for incurred, but unpaid, claim liability. This is an area where insurance companies profit. They overstate the reserves that they build into your premiums and then they earn investment income on the reserves. When you self-fund, you pay only for what you use.
Below is a recent case study
We received a broker of record letter from a growing company headquartered in Massachusetts. They were hovering at about 200 employees enrolled in their fully insured dental plan. After analyzing their historical dental claims experience, we saw an opportunity. After presenting the analysis and educating the employer on the limited amount of risk involved in switching to a self-funded program, the client decided to make the change.
After we had received 12 months of mature claims, we did a look back into the financial impact of the change. Had the client accepted what was historically a well-received “no change” fully insured dental renewal, they would have missed out on more than $90,000 added to their bottom line. Their employee contributions were competitive to begin with, so the employer held employee contributions flat and was able to reap the full financial reward.
This is just one example. I would not suggest that this is the norm, but savings of 10 percent are. If you are a mid-size employer with a fully insured dental plan, self-funding dental is a cost-savings opportunity you and your consultant should be monitoring at every renewal.
By Gary R Goodhile, Originally Published By United Benefit Advisors