by admin | Sep 15, 2017 | COBRA, ERISA, Group Benefit Plans
 The DOL issued guidance for employee benefit plans, plan sponsors, and employers located in a county identified for individual assistance by the Federal Emergency Management Agency (FEMA) due to Hurricane Harvey.
The DOL issued guidance for employee benefit plans, plan sponsors, and employers located in a county identified for individual assistance by the Federal Emergency Management Agency (FEMA) due to Hurricane Harvey.
Because plan participants and beneficiaries may have difficulty meeting deadlines for filing ERISA benefit claims and making COBRA elections, the DOL advised plan sponsors to “act reasonably, prudently, and in the interest of the workers and their families who rely on their health plans for their physical and economic well-being. Plan fiduciaries should make reasonable accommodations to prevent the loss of benefits in such cases and should take steps to minimize the possibility of individuals losing benefits because of a failure to comply with pre-established timeframes.”
The DOL acknowledged that group health plans may not be able to timely and fully comply with deadlines due to a physical disruption to a plan’s principal place of business. The DOL’s enforcement approach will emphasize compliance assistance, including grace periods and other relief as appropriate.
By Danielle Capilla
Originally Published By United Benefit Advisors

by admin | Sep 8, 2017 | Flexible Spending Accounts, Human Resources
 A dependent care flexible spending account (DCFSA) is a pre-tax benefit account used to pay for eligible dependent care services. The IRS determines which expenses are eligible for reimbursement and these expenses are defined by Internal Revenue Code §129 and the employer’s plan. Eligible DCFSA expenses include: adult day care center, before/after school programs, child care, nanny, preschool, and summer day camp. Day nursing care, nursing home care, tuition for kindergarten and above, food expenses, and overnight camp are ineligible expenses.
A dependent care flexible spending account (DCFSA) is a pre-tax benefit account used to pay for eligible dependent care services. The IRS determines which expenses are eligible for reimbursement and these expenses are defined by Internal Revenue Code §129 and the employer’s plan. Eligible DCFSA expenses include: adult day care center, before/after school programs, child care, nanny, preschool, and summer day camp. Day nursing care, nursing home care, tuition for kindergarten and above, food expenses, and overnight camp are ineligible expenses.
Qualifying Individuals
Only qualifying individuals are eligible for dependent care expenses. A qualifying individual is an individual who spends at least eight hours in the participant’s home.
Dependent care includes care for a child who is under the age of 13 and in the participant’s custody for more than half the year. Dependent care also includes care for a spouse or relative who is physically or mentally incapable of self-care and lives in the participant’s home.
If parents are divorced, then the child is a qualified dependent of the custodial parent. A non-custodial parent cannot be reimbursed under a DCFSA even if the parent claims the child as a tax dependent.
Contributing to a DCFSA
The election is the participant’s contribution amount, which is the amount the participant puts into a DCFSA at enrollment. Participants may change the amount of money to be withheld within a 31-day window after a qualifying event, such as marriage, birth or adoption of a child, dependent death, divorce, or change in employment. Participants may enroll in or renew their election in a DCFSA during open enrollment. Participation is not automatic. Participants must re-enroll every year by the enrollment date.
The employer determines the minimum election amount and the IRS determines the maximum election amount. The IRS sets the following annual contribution limits for a DCFSA:
- $2,500 per year for a married employee who files a separate tax return
- $5,000 per year for a married employee who files a joint tax return
- $5,000 per year for the head of household
- $5,000 per year for a single employee
Even though a different maximum contribution limit may apply depending on the employer’s plan, the maximum contribution cannot exceed the following earned income limitations:
- If you are single, the earned income limit is your salary, excluding contributions to your DCFSA.
- If you are married, the earned income limit is the lesser of: your salary, excluding contributions to your DCFSA, or your spouse’s salary.
All DCFSA contributions are subject to IRS use-it-or-lose-it rules, which means that unused funds within the plan year will be forfeited to the employer unless the employer’s plan offers a grace period extension. Some plans include a two-and-a-half-month grace period.
Participants must report their DCFSA contributions on their federal tax return along with the name, address, and Social Security number (if applicable) of the dependent care service provider.
Reimbursement Requests
A valid DCFSA claim will either have the dependent care provider certify the service by signing the claim form or have the participant provide an itemized statement from the dependent care provider that includes the following: service dates, dependent’s name, type of service, amount billed, and the provider’s name and address along with a completed claim form.
Participants should save supporting documentation related to their DCFSA expenses and claims because the IRS may request itemized receipts to verify the eligibility of their expenses.
By Danielle Capilla
Originally Published By United Benefit Advisors

by admin | Sep 6, 2017 | Compliance, HIPAA, Human Resources
 When it comes to Employee Assistance Programs, confidentiality is a concern for both employers and employees. As an employer, it is helpful to understand the terms and processes your EAP uses to keep information confidential and ensure that your employees and your workplace are safe.
When it comes to Employee Assistance Programs, confidentiality is a concern for both employers and employees. As an employer, it is helpful to understand the terms and processes your EAP uses to keep information confidential and ensure that your employees and your workplace are safe.
The Health Insurance Portability and Accountability Act (HIPAA) rules apply to EAPs and their affiliate providers. All information that is obtained during an EAP session is maintained in confidential files. The information remains confidential except in the following circumstances:
- An employee/client provides written permission/consent for the release of specific information. This can be done using a Consent to Inform or Release of Information form.
- The life or safety of the client or others is seriously threatened.
- Child abuse has occurred.
- EAP records are the subject of a court order (subpoena).
- Other disclosures required by applicable law.
Depending on the situation, an employee may use EAP services through a self-referral, guided-referral or mandated-referral
Voluntary or self-referrals are the most common. When an employee seeks EAP services voluntarily, all of the employee’s information, including whether he or she contacted the EAP or not, is confidential and cannot be released without written permission.
Guided referrals are an opportunity for the employer to encourage the employee to use EAP services when the employer senses there is a problem that needs to be addressed. This may occur when the employer identifies an employee who may be having personal or work-related difficulties but it is not to the point of mandating that the employee use an EAP. In the case of guided referrals, information disclosed by the employee is still kept confidential.
Mandatory or formal referrals usually occur when substance abuse or other behaviors are impacting productivity or safety. An employer’s policy may allow for putting the employee on a performance improvement plan and may even include a “last chance” agreement that states what an employee must do in order to keep their job. In these cases, employees are mandated by the employer to contact the EAP and a Release of Information is signed so the EAP can exchange information with the employer about employee attendance, compliance and recommendations.
In some cases, it may be advised to send the employee for a Fitness for Duty Evaluation or similar assessment to determine the employee’s ability to physically or mentally perform essential job duties, or assess for a potential threat of violence. These evaluations are performed by specially trained professionals and will come with an additional cost. If the employee has provided written consent, limited information may be released to the employer regarding the results of these evaluations.
By Kathryn Schneider
Originally Published By United Benefit Advisors

by admin | Aug 31, 2017 | Benefit Management, Flexible Spending Accounts

A health flexible spending account (FSA) is a pre-tax account used to pay for out-of-pocket health care costs for a participant as well as a participant’s spouse and eligible dependents. Health FSAs are employer-established benefit plans and may be offered with other employer-provided benefits as part of a cafeteria plan. Self-employed individuals are not eligible for FSAs.
Even though a health FSA may be extended to any employee, employers should design their health FSAs so that participation is offered only to employees who are eligible to participate in the employer’s major medical plan. Generally, health FSAs must qualify as excepted benefits, which means other nonexcepted group health plan coverage must be available to the health FSA’s participants for the year through their employment. If a health FSA fails to qualify as an excepted benefit, then this could result in excise taxes of $100 per participant per day or other penalties.
Contributing to an FSA
Money is set aside from the employee’s paycheck before taxes are taken out and the employee may use the money to pay for eligible health care expenses during the plan year. The employer owns the account, but the employee contributes to the account and decides which medical expenses to pay with it.
At the beginning of the plan year, a participant must designate how much to contribute so the employer can deduct an amount every pay day in accordance with the annual election. A participant may contribute with a salary reduction agreement, which is a participant election to have an amount voluntarily withheld by the employer. A participant may change or revoke an election only if there is a change in employment or family status that is specified by the plan.
Per the Patient Protection and Affordable Care Act (ACA), FSAs are capped at $2,600 per year per employee. However, since a plan may have a lower annual limit threshold, employees are encouraged to review their Summary Plan Description (SPD) to find out the annual limit of their plan. A participant’s spouse can put $2,600 in an FSA with the spouse’s own employer. This applies even if both spouses participate in the same health FSA plan sponsored by the same employer.
Generally, employees must use the money in an FSA within the plan year or they lose the money left in the FSA account. However, employers may offer either a grace period of up to two and a half months following the plan year to use the money in the FSA account or allow a carryover of up to $500 per year to use in the following year.
By Danielle Capilla
Originally Published By United Benefit Advisors

by admin | Aug 29, 2017 | ACA, Health Plan Benchmarking
 Small employers, those with fewer than 100 employees, have a reputation for not offering health insurance benefits that are competitive with larger employers, but new survey data from UBA’s Health Plan Survey reveals they are keeping pace with the average employer and, in fact, doing a better job of containing costs.
Small employers, those with fewer than 100 employees, have a reputation for not offering health insurance benefits that are competitive with larger employers, but new survey data from UBA’s Health Plan Survey reveals they are keeping pace with the average employer and, in fact, doing a better job of containing costs.
According to our new special report: “Small Businesses Keeping Pace with Nationwide Health Trends,” employees across all plan types pay an average of $3,378 toward annual health insurance benefits, with their employer picking up the rest of the total cost of $9,727. Among small groups, employees pay $3,557, with their employer picking up the balance of $9,474 – only a 5.3 percent difference.
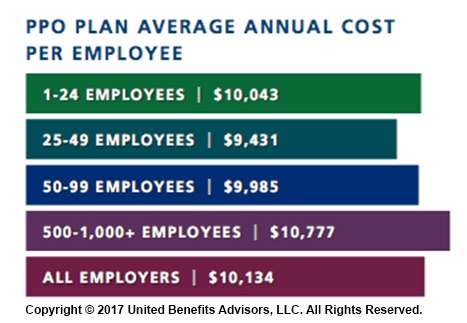
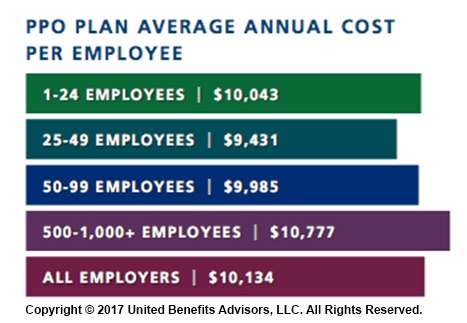
When looking at total average annual cost per employees for PPO plans, small businesses actually cut a better deal even compared to their largest counterparts—their costs are generally below average—and the same holds true for small businesses offering HMO and CDHP plans. (Keep in mind that relief such as grandmothering and the PACE Act helped many of these small groups stay in pre-ACA plans at better rates, unlike their larger counterparts.)
Think small businesses are cutting coverage to drive these bargains? Compared to the nations very largest groups, that may be true, but compared to average employers, small groups are highly competitive.
By Bill Olson
Originally Published By United Benefit Advisors

 The DOL issued guidance for employee benefit plans, plan sponsors, and employers located in a county identified for individual assistance by the Federal Emergency Management Agency (FEMA) due to Hurricane Harvey.
The DOL issued guidance for employee benefit plans, plan sponsors, and employers located in a county identified for individual assistance by the Federal Emergency Management Agency (FEMA) due to Hurricane Harvey.