by admin | Dec 12, 2017 | ACA, Benefit Management, Compliance, Group Benefit Plans, IRS
 Beginning in 2015, to comply with the Patient Protection and Affordable Care Act (ACA), “large” employers must offer their full-time employees health coverage, or pay one of two employer shared responsibility / play-or-pay penalties. The Internal Revenue Service (IRS) determines the penalty each calendar year after employees have filed their federal tax returns.
Beginning in 2015, to comply with the Patient Protection and Affordable Care Act (ACA), “large” employers must offer their full-time employees health coverage, or pay one of two employer shared responsibility / play-or-pay penalties. The Internal Revenue Service (IRS) determines the penalty each calendar year after employees have filed their federal tax returns.
In November 2017, the IRS indicated on its “Questions and Answers on Employer Shared Responsibility Provisions Under the Affordable Care Act” webpage that, in late 2017, it plans to issue Letter 226J to inform large employers of their potential liability for an employer shared responsibility payment for the 2015 calendar year.
The IRS’ determination of an employer’s liability and potential payment is based on information reported to the IRS on Forms 1094-C and 1095-C and information about the employer’s full-time employees that were received the premium tax credit.
The IRS will issue Letter 226J if it determines that, for at least one month in the year, one or more of a large employer’s full-time employees was enrolled in a qualified health plan for which a premium tax credit was allowed (and the employer did not qualify for an affordability safe harbor or other relief for the employee).
Letter 226J will include:
- A brief explanation of Section 4980H, the employer shared responsibility regulations
- An employer shared responsibility payment summary table that includes a monthly itemization of the proposed payment and whether the liability falls under Section 4980H(a) (the “A” or “No Offer” Penalty) or Section 4980H(b) (the “B” or “Inadequate Coverage” Penalty) or neither section
- A payment summary table explanation
- An employer shared responsibility response form (Form 14764 “ESRP Response”)
- An employee premium tax credit list (Form 14765 “Employee Premium Tax Credit (PTC) List”) which lists, by month, the employer’s assessable full-time employees and the indicator codes, if any, the employer reported on lines 14 and 16 of each assessable full-time employee’s Form 1095-C
- Actions the employer should take if it agrees or disagrees with Letter 226J’s proposed employer shared responsibility payment
- Actions the IRS will take if the employer does not timely respond to Letter 226J
- The date by which the employer should respond to Letter 226J, which will generally be 30 days from the date of the letter
- The name and contact information of the IRS employee to contact with questions about the letter
If an employer responds to Letter 226J, then the IRS will acknowledge the response with Letter 227 to describe further actions that the employer can take.
After receiving Letter 227, if the employer disagrees with the proposed or revised shared employer responsibility payment, the employer may request a pre-assessment conference with the IRS Office of Appeals. The employer must request the conference by the response date listed within Letter 227, which will be generally 30 days from the date of the letter.
If the employer does not respond to either Letter 226J or Letter 227, then the IRS will assess the proposed employer shared responsibility payment amount and issue a notice and demand for payment on Notice CP 220J.
Notice CP 220J will include a summary of the employer shared responsibility payment, payments made, credits applied, and the balance due, if any. If a balance is due, Notice CP 220J will instruct an employer how to make payment. For payment options, such as an installment agreement, employers should refer to Publication 594 “The IRS Collection Process.”
Employers are not required to make payment before receiving a notice and demand for payment.
The ACA prohibits employers from making an adverse employment action against an employee because the employee received a tax credit or subsidy. To avoid allegations of retaliation, as a best practice, employers who receive a Letter 226J should separate their employer shared responsibility penalty assessment correspondence from their human resources department and employees who have authority to make employment actions.
By Danielle Capilla
Originally Published By United Benefit Advisors

by admin | Dec 5, 2017 | Employee Benefits, Flexible Spending Accounts, IRS
 On November 2, 2017, House Republicans introduced a tax reform bill (H.R.1-115th Congress) called the “Tax Cuts and Jobs Act” that, if passed, would impact multiple aspects of the tax code. Many of these changes relate to employee benefit plans, particularly in relation to certain fringe benefits.
On November 2, 2017, House Republicans introduced a tax reform bill (H.R.1-115th Congress) called the “Tax Cuts and Jobs Act” that, if passed, would impact multiple aspects of the tax code. Many of these changes relate to employee benefit plans, particularly in relation to certain fringe benefits.
Dependent Care Accounts
A dependent care flexible spending account (DCFSA) is a pre-tax benefit account used to pay for eligible dependent care services. The IRS determines which expenses are eligible for reimbursement and these expenses are defined by Internal Revenue Code section 129 and the employer’s plan. Eligible DCFSA expenses include costs for adult day care centers, before and after school programs, child care, nannies, preschool, and summer day camp. Day nursing care, nursing home care, tuition for kindergarten and above, food expenses, and overnight camp are ineligible expenses. The employer determines the minimum election amount and the IRS determines the maximum election amount. The IRS sets the following annual contribution limits for a DCFSA:
- $2,500 per year for a married employee who files a separate tax return
- $5,000 per year for a married employee who files a joint tax return
- $5,000 per year for the head of household
- $5,000 per year for a single employee
The original version of the tax reform bill completely eliminated dependent care accounts. It is now reported that Representative Kevin Brady (R-Texas) has added an amendment to the bill that reverses the immediate repeal of DCFSAs, and would extend them for five more years.
Adoption Assistance
Employers may currently reimburse employees up to $13,570 (indexed) tax-free for qualified adoption expenses. This is eliminated in the bill.
Education Assistance
Employers may currently reimburse employees up to $5,250 on a tax-free basis for qualified education expenses. This is eliminated in the bill. Employers that are educational institutions can currently provide qualified tuition reductions to employees, their spouses, and dependents tax free, but this would be eliminated under the bill.
Employer Tax Deduction Impact
Under the proposed bill, employers’ corporate tax deduction credits for the following would be eliminated:
- Transportation fringe benefits
- On-premise athletic facilities
- Employer provided child care
The bill is now in markup, with the Ways and Means Committee working to draft a final bill for the House to vote on. If passed, it will be sent to the Senate to vote on.
By Danielle Capilla
Originally Published By United Benefit Advisors

by admin | Nov 30, 2017 | ACA, Employee Benefits, IRS
 On December 13, 2016, President Obama signed the 21st Century Cures Act (Cures Act) into law. The Cures Act provides a method for certain small employers to reimburse individual health coverage premiums up to a dollar limit through HRAs called “Qualified Small Employer Health Reimbursement Arrangements” (QSE HRAs). The provision went into effect on January 1, 2017. On October 31, 2017, the IRS released Notice 2017-67, providing guidance on the implementation and administration of QSE HRAs.
On December 13, 2016, President Obama signed the 21st Century Cures Act (Cures Act) into law. The Cures Act provides a method for certain small employers to reimburse individual health coverage premiums up to a dollar limit through HRAs called “Qualified Small Employer Health Reimbursement Arrangements” (QSE HRAs). The provision went into effect on January 1, 2017. On October 31, 2017, the IRS released Notice 2017-67, providing guidance on the implementation and administration of QSE HRAs.
Unless an employer meets all the requirements for offering a QSE HRA, previous IRS guidance prohibiting the reimbursement of individual premiums directly or indirectly, after- or pre-tax, through an HRA, a Section 125 plan, a Section 105 plan, or any other mechanism, remains in full effect. Reimbursing individual premiums in a non-compliant manner will subject an employer to a Patient Protection and Affordable Care Act (ACA) penalty of $100 a day per individual it reimburses, with the potential for other penalties based on the mechanism of the non-compliant reimbursement.
If an employer fails to meet the requirements of providing a QSE HRA, it will be subject to a penalty of $100 per day per affected person for being a non-compliant group health plan. An arrangement will be a group health plan that is not a QSE HRA if it:
- Is not provided by an eligible employer (such as an employer that offers another group health plan to its employees).
- Is not provided on the same terms to all eligible employees.
- Reimburses medical expenses without first requiring proof of minimum essential coverage (MEC).
- Provides a permitted benefit in excess of the statutory dollar limits.
An arrangement’s failure to be a QSE HRA will not cause any reimbursement of a properly substantiated medical expense that is otherwise excludable from income to be included in the employee’s income or wages. Furthermore, an arrangement designed to reimburse expenses other than medical expenses (whether or not also reimbursing medical expenses) is neither a QSE HRA nor a group health plan. Accordingly, all payments under such an arrangement are includible in the employee’s gross income and wages. An employer’s failure to timely provide a compliant written notice does not cause an arrangement to fail to be a QSE HRA, but instead results in the penalty of $50 per employee, not to exceed $2,500.
Answers to Top Three FAQs about QSE HRAs
1, Which employers may offer a QSE HRA?
Employers with fewer than 50 full-time and full-time equivalent employees (under ACA counting rules) that do not offer a group health plan. Employers that do not offer a group health plan, but offer a retiree-only plan to former employees may offer a QSE HRA.
2. Which employers may not offer a QSE HRA?
- Employers with 50 or more full-time and full-time equivalent employees (under ACA counting rules).
- Employers of any size that offer a group health plan, including plans that only provide excepted benefits, such as vision or dental benefits.
- Employers that provide current employees with access to money from health reimbursement arrangements (HRAs) offered in prior years (through a carry-over).
- Employers that offer employees access to carryover amounts in a flexible spending account (FSA).
3. What are the rules for employers in a controlled group?
- Employers with less than 50 full-time and full-time equivalent employees (under ACA counting rules) may offer QSE HRAs, with the headcount including all employees across an entire controlled group.
- If one employer within a controlled group offers a QSE HRA, it must be offered to all employees within the entire controlled group (or each employer must offer an identical QSE HRA).
BY Danielle Capilla
Originally Published By United Benefit Advisors

by admin | Nov 27, 2017 | ACA, COBRA, IRS
 Recently, the Internal Revenue Service (IRS) issued the instructions for Forms 1094/1095 for the 2017 tax year, announced PCORI fees for 2017-18, and announced cost-of-living adjustments for 2018. The IRS provided additional guidance on leave-based donation programs’ tax treatment and released an information letter on COBRA and Medicare. Here’s a recap of these actions for your reference.IRS Announces Cost-of-Living Adjustments for 2018
Recently, the Internal Revenue Service (IRS) issued the instructions for Forms 1094/1095 for the 2017 tax year, announced PCORI fees for 2017-18, and announced cost-of-living adjustments for 2018. The IRS provided additional guidance on leave-based donation programs’ tax treatment and released an information letter on COBRA and Medicare. Here’s a recap of these actions for your reference.IRS Announces Cost-of-Living Adjustments for 2018
The IRS released Revenue Procedures 2017-58 and Notice 2017-64 to announce cost-of-living adjustments for 2018. For example, the dollar limit on voluntary employee salary reductions for contributions to health flexible spending accounts (FSAs) is $2,650, for taxable years beginning with 2018.
Request UBA’s 2018 desk reference card with an at-a glance summary of the various limits.
IRS Announces PCORI Fee for 2017-18
The IRS announced the Patient-Centered Outcomes Research Institute (PCORI) fee for 2017-18. The fee is $1.00 per covered life in the first year the fee is in effect. The fee is $2.00 per covered life in the second year. In the third through seventh years, the fee is $2.00, adjusted for medical inflation, per covered life.
For plan years that end on or after October 1, 2016, and before October 1, 2017, the indexed fee is $2.26. For plan years that end on or after October 1, 2017, and before October 1, 2018, the indexed fee is $2.39.
For more information, view UBA’s FAQ on the PCORI Fee.
IRS Provides Additional Guidance on Leave-Based Donation Programs’ Tax Treatment
Last month, the IRS provided guidance for employers who adopt leave-based donation programs to provide charitable relief for victims of Hurricane and Tropical Storm Irma. This month, the IRS issued Notice 2017-62 which extends the guidance to employers’ programs adopted for the relief of victims of Hurricane and Tropical Storm Maria.
These leave-based donation programs allow employees to forgo vacation, sick, or personal leave in exchange for cash payments that the employer will make to charitable organizations described under Internal Revenue Code Section 170(c).
The employer’s cash payments will not constitute gross income or wages of the employees if paid before January 1, 2019, to the Section 170(c) charitable organizations for the relief of victims of Hurricane or Tropical Storm Maria. Employers do not need to include these payments in Box 1, 3, or 5 of an employee’s Form W-2.
IRS Releases Information Letter on COBRA and Medicare
The IRS released Information Letter 2017-0022 that explains that a covered employee’s spouse can receive COBRA continuation coverage for up to 36 months if the employee became entitled to Medicare benefits before employment termination. In this case, the spouse’s maximum COBRA continuation period ends the later of: 36 months after the employee’s Medicare entitlement, or 18 months (or 29 months if there is a disability extension) after the employment termination.
By Danielle Capilla
Originally Published By United Benefit Advisors

by admin | Nov 14, 2017 | ACA, Group Benefit Plans, Human Resources, IRS
 October was a busy month in the employee benefits world. President Trump announced a new Acting Secretary for the U.S. Department of Health and Human Services (HHS). Eric Hargan fills the position vacated by Tom Price, who resigned in late September 2017. The U.S. Department of Labor (DOL) issued a proposed rule to delay a disability claims procedure regulation’s applicability date and HHS released its proposed rule on benefits and payment parameters for 2019. The U.S. Department of the Treasury (Treasury) issued its Priority Guidance Plan for projects it intends to complete during the first half of 2018.
October was a busy month in the employee benefits world. President Trump announced a new Acting Secretary for the U.S. Department of Health and Human Services (HHS). Eric Hargan fills the position vacated by Tom Price, who resigned in late September 2017. The U.S. Department of Labor (DOL) issued a proposed rule to delay a disability claims procedure regulation’s applicability date and HHS released its proposed rule on benefits and payment parameters for 2019. The U.S. Department of the Treasury (Treasury) issued its Priority Guidance Plan for projects it intends to complete during the first half of 2018.
DOL Proposes Delay to Final Disability Claims Procedures Regulations’ Applicability Date
The DOL issued a proposed rule to delay the applicability date of its final rule that amends the claims procedure requirements applicable to ERISA-covered employee benefit plans that provide disability benefits. The DOL’s Fact Sheet contains a summary of the final rule’s requirements.
The DOL is delaying the applicability date from January 1, 2018, to April 1, 2018, to consider whether to rescind, modify, or retain the regulations and to give the public an additional opportunity to submit comments and data concerning the final rule’s potential impact.
CMS Releases 2019 Benefits Payment and Parameters Proposed Rule
The Centers for Medicare & Medicaid Services (CMS) released a proposed rule and fact sheet for the 2019 Benefit Payment and Parameters. The proposed rule is intended to increase individual market flexibility, improve program integrity, and reduce regulatory burdens associated with the Patient Protection and Affordable Care Act (ACA) in many ways, including updates and annual provisions to:
- Essential health benefits
- Small Business Health Options Program (SHOP)
- Special enrollment periods (SEPs)
- Exemptions
- Termination effective dates
- Medical loss ratio (MLR)
CMS usually finalizes the Benefit Payment and Parameters rule in the first quarter of the year following the proposed rule’s release. November 27, 2017, is the due date for public comments on the proposed rule.
Almost all the topics addressed in the proposed rule would affect the individual market and the Exchanges, particularly the Small Business Health Options Program (SHOP) Exchanges.
Of interest to small group health plans, CMS proposes to change how states will select essential health benefits benchmark plans. If CMS keeps this change in its final rule, then it will affect non-grandfathered small group health plans for benefit years 2019 and beyond.
Treasury Issues its Priority Guidance Plan
The Treasury issued its 2017-2018 Priority Guidance Plan that lists projects that it intends to complete by June 30, 2018, including:
- Guidance on issues related to the employer shared responsibility provisions
- Regulations regarding the excise tax on high cost employer-provided coverage (“Cadillac tax”)
- Guidance on Qualified Small Employer Health Reimbursement Arrangements (QSE HRAs)
By Danielle Capilla
Originally Published By United Benefit Advisors

by admin | Nov 9, 2017 | ACA, Human Resources, IRS

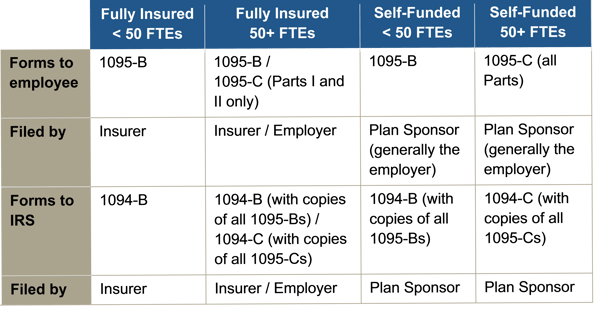
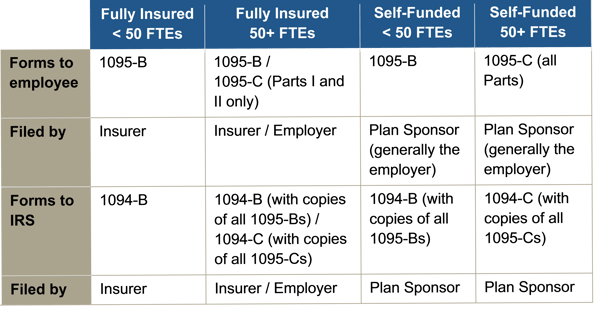
Instructions for both the 1094-B and 1095-B and the 1094-C and 1095-C were released, as were the forms for 1094-B, 1095-B, 1094-C, and 1095-C.
Reporting will be due early in 2018, based on coverage in 2017. For calendar year 2017, Forms 1094-C, 1095-C, 1094-B, and 1095-B must be filed by February 28, 2018, or April 2, 2018, if filing electronically. Statements to employees must be furnished by January 31, 2018. In late 2016, a filing deadline was provided for forms due in early 2017, however it is unknown if that extension will be provided for forms due in early 2018. Until employers are told otherwise, they should plan on meeting the current deadlines.
All reporting will be for the 2017 calendar year, even for non-calendar year plans.
The reporting requirements are in Sections 6055 and 6056 of the ACA. The major reporting requirements are:

 Beginning in 2015, to comply with the Patient Protection and Affordable Care Act (ACA), “large” employers must offer their full-time employees health coverage, or pay one of two employer shared responsibility / play-or-pay penalties. The Internal Revenue Service (IRS) determines the penalty each calendar year after employees have filed their federal tax returns.
Beginning in 2015, to comply with the Patient Protection and Affordable Care Act (ACA), “large” employers must offer their full-time employees health coverage, or pay one of two employer shared responsibility / play-or-pay penalties. The Internal Revenue Service (IRS) determines the penalty each calendar year after employees have filed their federal tax returns.