by admin | Jul 16, 2018 | Health & Wellness, Hot Topics
 Don’t lie–we ALL love gadgets. From the obscure (but hilariously reviewed on Amazon) Hutzler 571 Banana Slicer to the latest iteration of the Apple empire. Gadgets and technology can make our lives easier, make processes faster, and even help us get healthier. Businesses are now using the popularity of wearable technology to encourage employee wellness and increase productivity and morale.
Don’t lie–we ALL love gadgets. From the obscure (but hilariously reviewed on Amazon) Hutzler 571 Banana Slicer to the latest iteration of the Apple empire. Gadgets and technology can make our lives easier, make processes faster, and even help us get healthier. Businesses are now using the popularity of wearable technology to encourage employee wellness and increase productivity and morale.
According to a survey cited on Huffington Post, “82% of wearable technology users in American said it enhanced their lives in one way or another.” How so? Well, in the instance of health and wellness, tech wearers are much more aware of how much, or how little, they are moving throughout the day. We know that our sedentary lifestyles aren’t healthy and can lead to bigger health risks long term. Obesity, heart disease, high blood pressure, and Type 2 Diabetes are all side effects of this non-active lifestyle. But, these are all side effects that can be reversed with physically getting moving. Being aware of the cause of these problems helps us get motivated to work towards a solution.
Fitbit, Apple Watch, Pebble, and Jawbone UP all have activity tracking devices. Many companies are offering incentives for employees who work on staying fit and healthy by using this wearable technology. For example, BP Oil gave employees a free Fitbit in exchange for them tracking their annual steps. Those BP employees who logged 1 million steps in a year were given lower insurance premiums. These benefits for the employee are monetary but there are other pros to consider as well. The data collected with wearable technology is very accurate and can help the user when she goes to her physician for an ailment. The doctor can look at this data and it can help connect the dots with symptoms and then assist the provider with a diagnosis.
So, what are the advantages to the company who creates wellness programs utilizing wearable technology?
- Job seekers have said that employee wellness programs like this are very attractive to them when looking for a job.
- Millennials are already wearing these devices and say that employers who invest in their well-being increases employee morale.
- Employee healthcare costs are reduced.
- Improved productivity including fewer disruptions from sick days.
The overall health and fitness of the company can be the driving force behind introducing wearable technology in a business but the benefits are so much more than that. Morale and productivity are intangible benefits but very important ones to consider. All in all, wearable technology is a great incentive for adopting healthy lifestyles and that benefits everyone—employee AND employer.

by admin | Mar 5, 2018 | Health & Wellness, Human Resources
 This year’s flu season is a rough one. Although the predominant strains of this year’s influenza viruses were represented in the vaccine, they mutated, which decreased the effectiveness of the immunization. The flu then spread widely and quickly, and in addition, the symptoms were severe and deadly. The U.S. Centers for Disease Control and Prevention (CDC) reported that the 2017 – 2018 flu season established new records for the percentage of outpatient visits related to flu symptoms and number of flu hospitalizations.
This year’s flu season is a rough one. Although the predominant strains of this year’s influenza viruses were represented in the vaccine, they mutated, which decreased the effectiveness of the immunization. The flu then spread widely and quickly, and in addition, the symptoms were severe and deadly. The U.S. Centers for Disease Control and Prevention (CDC) reported that the 2017 – 2018 flu season established new records for the percentage of outpatient visits related to flu symptoms and number of flu hospitalizations.
Younger, healthy adults were hit harder than is typical, which had impacts on the workplace. In fact, Challenger, Gray & Christmas, Inc. recently revised its estimates on the impact of this flu season on employers, raising the cost of lost productivity to over $21 billion, with roughly 25 million workers falling ill.
Fortunately, the CDC is reporting that it looks like this season is starting to peak, and while rates of infection are still high in most of the country, they are no longer rising and should start to drop. What can you do as an employer to keep your business running smoothly for the rest of this flu season and throughout the next one?
- Help sick employees stay home. Consider that sick employees worried about their pay, unfinished projects and deadlines, or compliance with the company attendance policy may feel they need to come to work even if they are sick. Do what you can to be compassionate and encourage them to stay home so they can get better as well as protect their co-workers from infection. In addition, make sure your sick leave policies are compliant with all local and state laws, and communicate them to your employees. Be clear with the expectation that sick employees not to report to work. For employees who feel well enough to work but may still be contagious, encourage them to work remotely if their job duties will allow. Be consistent in your application of your attendance and remote work rules.
- Know the law. Although the flu is generally not serious enough to require leaves of absence beyond what sick leave or PTO allow for, in a severe season, employees may need additional time off. Consider how the federal Family and Medical Leave Act (FMLA), state leave laws, and the Americans with Disabilities Act (ADA) may come into play for employees who have severe cases of the flu, complications, or family members who need care.
- Be flexible. During acute flu outbreaks, schools or daycare facilities may close, leaving parents without childcare. Employees may also need to be away from the workplace to provide care to sick children, partners, or parents. Examine your policies to see where you can provide flexibility. Look for opportunities to cross-train employees on each other’s essential duties so their work can continue while they are out.
- Keep it clean. Direct cleaning crews to thoroughly disinfect high-touch areas such as doorknobs, kitchen areas, and bathrooms nightly. Provide hand sanitizer in common areas and encourage frequent handwashing. Keep disinfecting wipes handy for staff to clean their personal work areas with.
- Limit exposure. Avoid non-essential in-person meetings and travel that can expose employees to the flu virus. Rely on technology such as video conferencing, Slack, Skype, or other platforms to bring people together virtually. Consider staggering work shifts if possible to limit the number of people in the workplace at one time.
- Focus on wellness. Offer free or low-cost flu shots in the workplace. If your company provides snacks or meals for employees, offer healthier options packed with nutrients.
Get it all
AGENCY RESOURCES: Get the latest weekly flu stats from the CDC. Learn more about how the FMLA and ADA may be used during pandemic flu from the U.S. Department of Labor.
By Rachel Sobel
Originally published by www.ThinkHR.com

by admin | Oct 16, 2017 | Health & Wellness, Hot Topics, Human Resources
 There are places where you expect things to be noisy, such as a rock concert, and places where you expect it to be quiet, like an office. And while nobody likes being “shushed,” there are few things more annoying than trying to work when someone else is talking in the background.
There are places where you expect things to be noisy, such as a rock concert, and places where you expect it to be quiet, like an office. And while nobody likes being “shushed,” there are few things more annoying than trying to work when someone else is talking in the background.
The ‘80s music group ‘Til Tuesday said it best: “Hush hush, keep it down now, voices carry.” An article in Human Resource Executive Online titled, “A Not-So-Quiet Little Problem: Noise!,” points out the current problem of modern, open offices—NOISE. When offices had doors, or at least cubicles, along with sound-absorbing carpeting and ceiling tiles, background noise wasn’t such a problem. Now, however, offices are wide open with nothing to block sound waves. Combine that with hardwood, or concrete floors, lots of glass and tall, echoing ceilings, and you’ve got the perfect storm for noise pollution.
Forward-thinking, or technology companies especially like open offices, and you can imagine what it sounds like with people talking on the phone, banging away at their keyboards, and conversing with each other. According to the article, nobody considers the acoustics of a room. They look at how beautiful, modern, and spacious it is. Then, once the room is filled with busy employees, the shock of its lack of tranquility sets in.
Employees become distracted by the noise, which in turn leads to reduced productivity. You can tell a lot about the noise level of an office by how many employees are wearing headphones. For workers to feel “healthy” at work, noise is a major factor, along with air quality and temperature.
There are many ways to fix a noisy office if you follow the A, B, Cs—absorb, block, cover. Materials can be placed to absorb noise, walls or furniture can be positioned to block noise, and there are electronic devices that use counter-measures to cover noise. The industry, office layout, and other factors will influence the choice of the best solution to mitigate noise. One thing is certain: when choosing a new office, or remodeling an existing one, it’s best to factor in a room’s acoustics along with its aesthetics.
By Geoff Mukhtar
Originally posted by www.UBABenefits.com

by admin | Sep 22, 2017 | Employee Benefits, Health & Wellness
 On August 22, 2017, the United States District Court for the District of Columbia held that the U.S. Equal Employment Opportunity Commission (EEOC) failed to provide a reasoned explanation for its decision to adopt 30 percent incentive levels for employer-sponsored wellness programs under both the Americans with Disabilities Act (ADA) rules and Genetic Information Nondiscrimination Act (GINA) rules.
On August 22, 2017, the United States District Court for the District of Columbia held that the U.S. Equal Employment Opportunity Commission (EEOC) failed to provide a reasoned explanation for its decision to adopt 30 percent incentive levels for employer-sponsored wellness programs under both the Americans with Disabilities Act (ADA) rules and Genetic Information Nondiscrimination Act (GINA) rules.
The court declined to vacate the EEOC’s rules because of the significant disruptive effect it would have. However, the court remanded the rules to the EEOC for reconsideration.
Based on the recent court decision to require the EEOC to reconsider its wellness program rules, does this mean that the EEOC rules no longer apply to employer wellness programs? No. For now, the current EEOC rules apply to employer wellness programs. However, employers should stay informed on the status of the EEOC’s reconsideration of the wellness program rules so that employers can change their wellness programs’ design, if necessary, to comply with new EEOC rules.
According to UBA’s free special report, “How Employers Use Wellness Programs,” 67.7 percent of employers who offer wellness programs have incentives built into the program, an increase of 8.5 percent from four years ago. Incentives are the most prevalent in the Central U.S. (76.1 percent), among employers with 500 to 999 employees (83.2 percent), and in the finance, insurance, and real estate industries (74.7 percent). The West offers the fewest incentives, with only 48.3 percent of their plans having rewards.
Across all employers, slightly more (45.4 percent) prefer wellness incentives in the form of cash toward premiums, 401(k)s, flexible spending accounts (FSAs), etc., versus health club dues and gift cards (40 percent). But among larger employers (500 to 1,000+ employees) cash incentives are more heavily preferred (63.2 percent) over gift certificates and health club dues (33.7 percent). Conversely, smaller employers (1 to 99 employees) prefer health club-related incentives (nearly 40 percent) versus cash (25 percent).
Download our free (no form!) special report, “How Employers Use Wellness Programs,” for more information on regional, industry and group size based trends surrounding prevalence of wellness programs, carrier vs. independent providers, and wellness program components.
For comprehensive information on designing wellness programs that create lasting change, download UBA’s whitepaper: “Wellness Programs — Good for You & Good for Your Organization”.
To understand legal requirements for wellness programs, request UBA’s ACA Advisor, “Understanding Wellness Programs and Their Legal Requirements,” which reviews the five most critical questions that wellness program sponsors should ask and work through to determine the obligations of their wellness program under the ACA, HIPAA, ADA, GINA, and ERISA, as well as considerations for wellness programs that involve tobacco use in any way.
By Danielle Capilla
Originally Published By United Benefit Advisors

by admin | Aug 15, 2017 | Compliance, Health & Wellness
 Where to Start?
Where to Start?
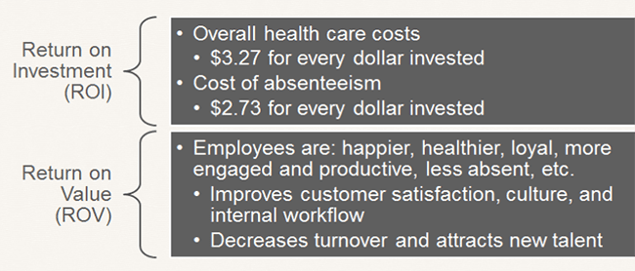
First, expand the usual scope of wellness activity to well-BEING. Include initiatives that support more than just physical fitness, such as career growth, social needs, financial health, and community involvement. By doing this you increase your chances of seeing a return on investment (ROI) and a return on value (ROV). Qualitative results of a successful program are just as valuable as seeing a financial impact of a healthier population.
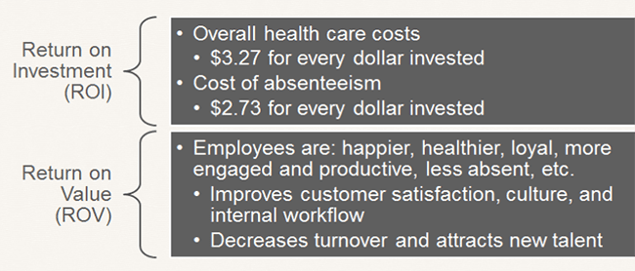
Source: Katherine Baicker, David Cutler, and Zirui Song, “Workplace Wellness Programs Can Generate Savings,” Health Affairs, February 2010, 29(2): pp 304-311
To create a corporate culture of well-being and ensure the success of your program, there are a few important steps.
- Leadership Support: Programs with leadership support have the highest level of participation. Gain leadership support by having them participate in the programs, give recognition to involved employees, support employee communication, allow use of on-site space, approve of employees spending time on coordinating and facilitating initiatives, and define the budget. Even though you do not need a budget to be successful.
- Create a Committee or Designate a Champion: Do not take this on by yourself. Create a well-being committee, or identify a champion, to share the responsibility and necessary actions of coordinating a program.
- Strategic Plan: Create a three-year strategic plan with a mission statement, budget, realistic goals, and measurement tools. Creating a plan like this takes some work and coordination, but the benefits are significant. You can create a successful well-being program with little to no budget, but you need to know what your realistic goals are and have a plan to make them a reality.
- Tools and Resources: Gather and take advantage of available resources. Tools and resources from your broker and/or carrier can help make managing a program much easier. Additionally, an employee survey will help you focus your efforts and accommodate your employees’ immediate needs.
How to Remain Compliant?
As always, remaining compliant can be an unplanned burden on employers. Whether you have a wellness or well-being program, each has their own compliance considerations and requirements to be aware of. However, don’t let that stop your organization from taking action.
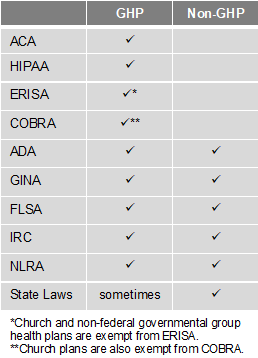
There are two types of programs – Group Health Plans (GHP) and Non-Group Health Plans (Non-GHP). The wellness regulations vary depending on the type of employer and whether the program is considered a GHP or Non-GHP.
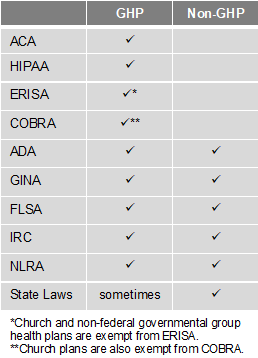
Employers looking to avoid some of the compliance burden should design their well-being program to be a Non-GHP. Generally, a well-being program is Non-GHP if it is offered to all employees regardless of their enrollment in the employer’s health plan and does not provide or pay for “medical care.” For example, employees receive $100 for attending a class on nutrition. Here are some other tips to keep your well-being program Non-GHP:
- Financial: Do not pay for medical services (e.g., flu shots, biometric screenings, etc.) or provide medical care. Financial incentives or rewards must be taxed. Do not provide premium discounts or surcharges.
- Voluntary Participation: Include all employees, but do not mandate participation. Make activities easily accessible to those with disabilities or provide a reasonable alternative. Make the program participatory (i.e., educational, seminars, newsletters) rather than health-contingent (i.e., require participants to get BMI below 30 or keep cholesterol below 200). Do not penalize individuals for not participating.
- Health Information: Do not collect genetic data, including family medical history. Any medical records, or information obtained, must be kept confidential. Avoid Health Risk Assessments (i.e. health surveys) that provide advice and analysis with personalized coaching or ask questions about genetics/family medical history.
By Hope DeRocha
Originally Posted By www.ubabenefits.com
by admin | Aug 7, 2017 | ACA, Employee Benefits, Health & Wellness
Preexisting conditions. While it’s no doubt this term has been a hot topic in recent months—and notably misconstrued—one thing has not changed; insurers cannot deny coverage to anyone with a preexisting condition. Now that House Resolution 1628 has moved to the Senate floor, what can employers and individuals alike expect? If passed by the Senate as is and signed into law; some provisions will take place as early as 2019—possibly 2018 for special enrollment cases. It’s instrumental for companies to gear up now with a plan on how to tackle open enrollment; regardless of whether your company offers medical coverage or not.
Under the current proposed American Health Care Act (AHCA) insurance companies can:
- Price premiums based on health care status/age. The AHCA will provide “continuous coverage” protections to guarantee those insured are not charged more than the standard rate as long as they do not have a break in coverage. However, insurers will be allowed to underwrite certain policies for those that do lapse—hence charging up to 30% more for a preexisting condition if coverage lapses for more than 63 days. This is more common than not, especially for those who are on a leave of absence for illness or need extensive treatment. In addition, under current law, insurers are only allowed to charge individuals 50 and older 3 times as much than those under this age threshold. This ratio will increase 5:1 under AHCA.
- Under the ACA’s current law employers must provide coverage for 10 essential health care benefits. Under AHCA, beginning as early as 2020, insurers will allow states to mandate what they consider essential benefit requirements. This could limit coverage offered to individuals and within group plans by eliminating high cost care like mental health and substance abuse. Not that it’s likely, but large employers could eventually opt out whether they want to provide insurance and/or choose the types of coverage they will provide to their employees.
It’s important to note that states must apply for waivers to increase the ratio on insurance premiums due to age, and determine what they will cover for essential health benefits. In order to have these waivers granted, they would need to provide extensive details on how doing so will help their state and the marketplace.
So what can employers do moving forward? It’s not too soon to think about changing up your benefits package as open enrollment approaches, and educating yourself and your staff on AHCA and what resources are out there if you don’t offer health coverage.
- Make a variety of supplemental tools available to your employees. Anticipate the coming changes by offering or adding more supplemental insurance and tools to your benefits package come open enrollment. Voluntary worksite benefits, such as Cancer, Critical Illness, and Accident Insurance handle a variety of services at no out-of-pocket cost to the employer. HSA’s FSA’s and HRA’s are also valuable supplemental tools to provide your employees if you’re able to do so. Along with the changes listed above, the AHCA has proposed to also increase the contribution amounts in these plans and will allow these plans to cover Over-the-Counter (OTC) medications.
- Continue to customize wellness programs. Most companies offer wellness programs for their employees. Employers that provide this option should continue advancing in this area. Addressing the specific needs of your employees and providing wellness through various platforms will result in the greatest return on investment; and healthier employees to boot. Couple this with frequent evaluations from your staff on your current program to determine effectiveness and keep your wellness programs on point.
- Educate, educate, educate—through technology. Regardless if you employ 10 or 10,000, understanding benefit options is vital for your employees; what you have to offer them and what they may need to know on their own. Digital platforms allow individuals to manage their healthcare benefits and stay in the know with valuable resources at their fingertips. There’s no limit on the mediums available to educate your employees on upcoming changes. Partnering with a strong benefit agency to maximize these resources and keep your employees “in the know” during a constantly changing insurance market is a great way to start.

 Don’t lie–we ALL love gadgets. From the obscure (but hilariously reviewed on Amazon) Hutzler 571 Banana Slicer to the latest iteration of the Apple empire. Gadgets and technology can make our lives easier, make processes faster, and even help us get healthier. Businesses are now using the popularity of wearable technology to encourage employee wellness and increase productivity and morale.
Don’t lie–we ALL love gadgets. From the obscure (but hilariously reviewed on Amazon) Hutzler 571 Banana Slicer to the latest iteration of the Apple empire. Gadgets and technology can make our lives easier, make processes faster, and even help us get healthier. Businesses are now using the popularity of wearable technology to encourage employee wellness and increase productivity and morale.