by admin | Jun 21, 2017 | Benefit Management, COBRA
 The Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) requires employers to offer covered employees who lose their health benefits due to a qualifying event to continue group health benefits for a limited time at the employee’s own cost. Per regulation, qualifying events are specific events that cause or trigger an individual to lose health coverage. The type of qualifying event determines who the qualified beneficiaries are and the maximum length of time a plan must offer continuation coverage. A group health plan may provide longer periods of continuation coverage beyond the maximum 18 or 36 months required by law.
The Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) requires employers to offer covered employees who lose their health benefits due to a qualifying event to continue group health benefits for a limited time at the employee’s own cost. Per regulation, qualifying events are specific events that cause or trigger an individual to lose health coverage. The type of qualifying event determines who the qualified beneficiaries are and the maximum length of time a plan must offer continuation coverage. A group health plan may provide longer periods of continuation coverage beyond the maximum 18 or 36 months required by law.
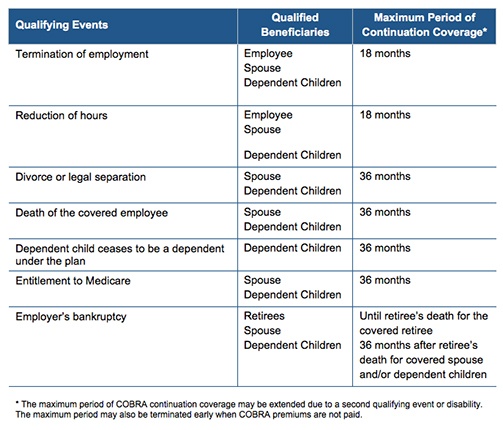
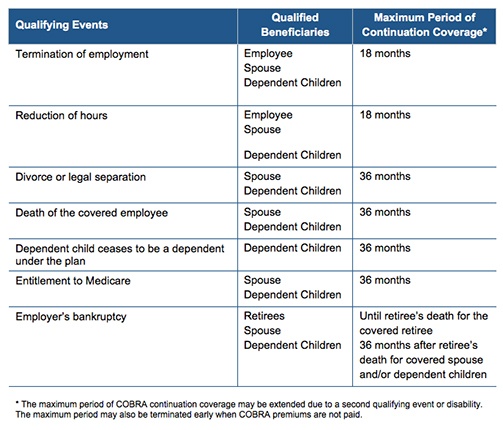
There are seven triggering events that are qualifying events for COBRA coverage if they result in loss of coverage for the qualified beneficiaries, which may include the covered employee, the employee’s spouse, and dependent children.
The following quick reference chart indicates the qualifying event, the individual who is entitled to elect COBRA, and the maximum length of COBRA continuation coverage.
By Danielle Capilla
Originally Posted By www.ubabenefits.com

by admin | Jun 1, 2017 | Benefit Management, ERISA, HSA/HRA, IRS
 Certain small employers have the option to reimburse individual health coverage premiums up to a dollar limit through Qualified Small Employer Health Reimbursement Arrangements (QSE HRAs) under the 21st Century Cures Act (Cures Act).
Certain small employers have the option to reimburse individual health coverage premiums up to a dollar limit through Qualified Small Employer Health Reimbursement Arrangements (QSE HRAs) under the 21st Century Cures Act (Cures Act).
The Cures Act amends the Employee Retirement Income Security Act of 1974 (ERISA) to exclude QSE HRAs from the ERISA definition of group health plan; however, the Cures Act does not specifically exclude QSE HRAs from the rest of ERISA.
Small employers that plan to offer QSE HRAs should be cautious before presuming that ERISA would not apply to a reimbursement arrangement. Because QSE HRAs are new, the issue of whether the remainder of ERISA applies to QSE HRAs remains undetermined by an administrative agency or court. In consideration of the limited ERISA group health definition exclusion and the law’s legislative history, a risk-averse small employer should treat a QSE HRA as an employee welfare benefit plan covered under ERISA and comply with applicable ERISA requirements such as having a written plan document and summary plan description as well as following ERISA’s fiduciary and other rules.
Request UBA’s Compliance Advisor, “Qualified Small Employer Health Reimbursement Arrangements and ERISA” for a discussion of ERISA’s definitions of “group health plan,” as well as the law’s legislative history governing exclusions. A small employer who intends to offer a QSE HRA without complying with ERISA’s employee welfare benefit plan requirements should consult with its attorney before proceeding.
By Danielle Capilla
Originally Posted By www.ubabenefits.com

by admin | May 23, 2017 | Benefit Management, Health & Wellness
 Your wellness program seems to have it all – biometric screenings, lunch and learns, and weight loss challenges. So, why do you struggle with engagement, or to see any real results? While traditional wellness components are still a large part of plans today, emerging trends, coupled with generational differences, make for challenges when designing an impactful program.
Your wellness program seems to have it all – biometric screenings, lunch and learns, and weight loss challenges. So, why do you struggle with engagement, or to see any real results? While traditional wellness components are still a large part of plans today, emerging trends, coupled with generational differences, make for challenges when designing an impactful program.
As wellness programs begin to be viewed as a part of the traditional benefits package, the key differentiator is creating a culture and environment that supports overall health and well-being. Visible engagement and support from front-line and senior leadership drives culture change. By prioritizing health through consistent communication, resource allocation, personnel delegation, and role modeling/personal health promotion practices, employers gain the trust of their employees and develop an environment situated around wellness. When employees recognize the importance of wellness in the overall company strategy and culture, and feel supported in their personal goals, healthy working environments begin to develop, resulting in healthier employees.
Looking beyond traditional wellness topics and offering programs that meet the goals of your employees also leads to higher engagement. The American Heart Association CEO Roundtable Employee Health Survey 2016 showed improving financial health, getting more sleep, and reducing stress levels are key focus areas for employees as part of overall wellness. More so, employees see the benefits of unplugging and mentoring, two new topics in the area of overall well-being. While most employers feel their employees are over surveyed, completing an employee needs or preference survey will ensure your programs align with your employees’ health and wellness goals – ultimately leading to better engagement.
Wellness programs are not immune to generational differences, like most other facets of business. While millennials are most likely to participate and report that programs had an overall impact, they prefer the use of apps and trackers along with social strategies and team challenges. Convenience and senior level support are also important within this group. Generation X and baby boomers show more skepticism toward wellness programs, but are more likely to participate when the programs align with their personal goals. Their overall top health goal is weight loss. Ultimately, addressing the specific needs of your member population and providing wellness through various modalities will result in the greatest reward of investment.
Evaluation and data are the lynchpins that hold a successful program together. Consistent evaluation of the effectiveness of programs to increase participation, satisfaction, physical activity, and productivity – all while reducing risk factors – allow us to know if our programs are hitting the mark and allow for additional tailoring as needed.
By Jennifer Jones
Originally Posted By www.ubabenefits.com

by admin | May 19, 2017 | Benefit Management, HSA/HRA
 In a world of insurance and acronyms, the term “HRA” is thrown around a lot, but it has a variety of meanings.
In a world of insurance and acronyms, the term “HRA” is thrown around a lot, but it has a variety of meanings.
HRA can mean health reimbursement account, heath reimbursement arrangement, or health risk assessment, and all of those mean something different. I want to be clear that in the following article I am going to be discussing the use of health reimbursement accounts with fully insured health plans. We can leave the other meanings of HRA for another time.
An HRA can be “wrapped” with a high-deductible, fully insured health plan and this can lead to savings for an employer over offering a traditional health plan with a lower deductible.
Offering a high-deductible health plan and self-funding, the first $2,000, or $3,000, in claims on behalf of the employees can translate to significant savings because the employer is taking on that initial risk instead of the insurance carrier. Unlike a consumer-driven health plan (CDHP) that has a high deductible and can be paired with a health savings account (HSA) where an employer can contribute funds to an employee’s HSA account that can be used to pay for qualified medical expenses, an employer only has to pay out of the HRA if there is a claim.
With an HSA that is funded by the employer, the money goes into the HSA for their employees and then those funds are “owned” by the employee. The employer never sees it again. Under an HRA, if there are no claims, or not a high number of claims, the employer keeps those unused dollars in their pocket.
An HRA component to a health plan is subject to ERISA and non-discrimination rules, meaning everyone that is eligible should be offered the plan, and the benefits under the HRA should be the same for everyone enrolled. It is advisable that an HRA be administered by a third-party that pays the claims to the providers, or reimburse plan enrollees under the terms of the plan, in order to keep employees’ and their dependents’ medical information private from the employer as to avoid potential discrimination.
The HRA component of a health plan is essentially self-funded by the employer, which gives the employer a lot of flexibility and can be tailored to their specific needs or desired outcomes. The employer can choose to fund claims after the employee pays the first few hundred dollars of their deductible instead of the employer paying the claims that are initially subject to the high deductible. An employer can have a step arrangement, for example, the employer pays the first $500, the employee the second $500, the employer pays the next $500, and the employee pays the final $500 of a $2,000 deductible.
If an employer has a young population that is healthy, they may want to use the HRA to pay for emergency room visits and hospital in-patient stays, but not office visits so they can help protect their employees from having to pay those “large ticket items,” but not blow their budget. While an employer with a more seasoned staff, or diverse population, may want to include prescription drugs as a covered benefit under the HRA, as well as office visits, hospital in-patient stays, outpatient surgery, etc. Or, if an employer needs to look at cost-saving measures, they may want to exclude prescriptions from being eligible under the HRA.
Keep in mind, all of these services are essential health benefits and would be covered by the insurance carrier under the terms of the contract, but an employer can choose not to allow the HRA to be used to pay for such services, leaving the enrollee to pay their portion of the claims. In any case, the parameters of what is eligible for reimbursement from the HRA is decided and outlined at the beginning of the plan year and cannot be changed prior to the end of the plan year.
If you are thinking about implementing a high-deductible health plan with an HRA for your employees, be sure you are doing it as a long-term strategy. As is the case with self-funding, you are going to have good years and bad years. On average, a company will experience a bad, or high claims, year out of every four to five years. So, if you implement your new plan and you have a bad year on the first go-round, don’t give up. Chances are the next year will be better, and you will see savings over your traditional low-deductible plan options.
With an HRA, you cap the amount you are going to potentially spend for each enrollee, per year. So, you know your worst-case scenario. While it is extremely unlikely that every one of your employees will use the entire amount allotted to them, it is recommended that you can absorb or handle the worst case scenario. Don’t bite off more than you can chew!
HRA administrators usually charge a monthly rate per enrollee for their services, and this should be accounted for in the budgeting process. Different HRA third-party administrators have different claims processes, online platforms, debit cards, and business hours. Be sure to use one that offers the services that you want and are on budget.
Another aspect of offering a high-deductible plan with an HRA that is often overlooked is communication. If an employee does not know how to utilize their plan, it can create confusion and anger, which can hurt the overall company morale. The plan has to be laid out and explained in a way that is clear, concise, and easy to understand.
In some cases, the HRA is administered by someone other than the insurance carrier, and the plan administrator has to make sure they enroll all plan enrollees with the carrier and the third-party administrator.
The COBRA administrator also has to offer the HRA as part of the COBRA package, and the third-party administrator must communicate the appropriate premium for the HRA under COBRA. Most COBRA enrollees will not choose to enroll in the HRA with their medical plan, as they are essentially self-funding their deductible and plan costs through the HRA instead of paying them out of their pocket, but many plan administrators make the mistake of not offering the HRA under COBRA, as it is mandated by law.
Offering a high-deductible plan with an HRA is a way for small employers to save over offering a low-deductible health plan, and can be a way for an employer to “test the waters” to see if they may want to move to a self-funded plan, or level-funded plan, in the future.
By Elizabeth Kay
Originally Posted By www.ubabenefits.com
by admin | May 3, 2017 | ACA, Benefit Management
 A Summary of Benefits and Coverage (SBC) is four page (double-sided) communication required by the federal government. It must contain specific information, in a specific order, and with a minimum size type, about a group health benefit’s coverage and limitations. If an employer providing an SBC is a covered entity under the Section 1557 of the Patient Protection and Affordable Care Act (ACA), additional requirements apply.
A Summary of Benefits and Coverage (SBC) is four page (double-sided) communication required by the federal government. It must contain specific information, in a specific order, and with a minimum size type, about a group health benefit’s coverage and limitations. If an employer providing an SBC is a covered entity under the Section 1557 of the Patient Protection and Affordable Care Act (ACA), additional requirements apply.
On April 6, 2016, the Centers for Medicare and Medicaid Services (CMS), the Department of Labor (DOL), and the Department of the Treasury issued the final 2017 summary of benefits and coverage (SBC) template, group and individual market SBC instructions, uniform glossary of coverage and medical terms, a coverage example calculator, and calculator instructions.
The SBC is to be used by all health plans, including individual, small group, and large group; insured and self-funded; grandfathered, transitional, and ACA compliant. The new SBC must be used for plan years with open enrollment periods beginning after April 1, 2017. It will not be used for marketplace plans for the 2017 coverage year.
For fully insured plans, the insurer is responsible for providing the SBC to the plan administrator (usually this is the employer). The plan administrator and the insurer are both responsible for providing the SBC to participants, although only one of them actually has to do this.
For self-funded plans, the plan administrator is responsible for providing the SBC to participants. Assistance may be available from the plan administrator’s TPA, advisor, etc., but the plan administrator is ultimately responsible. (The plan administrator is generally the employer, not the claims administrator.)
Changes
The template includes a new “important question” that asks “Are there services covered before you meet your deductible?” and requires family plans to disclose whether or not the plan has embedded deductibles or out-of-pocket limits. This is reported in the “Why This Matters” column in relation to the question “what is the overall deductible?” and plans must list “If you have other family members on the policy, they have to meet their own individual deductible until the overall family deductible has been met” or alternatively, “If you have other family members on the policy, the overall family deductible must be met before the plan begins to pay.”
Tiered networks must be disclosed and the question “Will you pay less if you use a network provider?” is now included. The SBC also includes language that warns participants that they could receive out-of-network providers while they are in an in-network facility. The SBC also indicates that a consumer could receive a “balance bill” from an out-of-network provider.
The “explanatory coverage page” was dropped from the template.
The coverage examples provided clarify the “having a baby” example and the “managing type 2 diabetes” example, in addition to providing a third example of “dealing with a simple fracture.” The coverage example must be calculated assuming that a participant does not earn wellness credits or participate in an employer’s wellness program. If the employer has a wellness program that could reduce the employee’s costs, the employer must include the following language: “These numbers assume the patient does not participate in the plan’s wellness program. If you participate in the plan’s wellness program, you may be able to reduce your costs. For more information about the wellness program, please contact: [insert].”
The column for “Limitations, Exceptions, & Other Important Information” must contain core limitations, which include:
- When a service category or a substantial portion of a service category is excluded from coverage (that is, the column should indicate “brand name drugs excluded” in health benefit plans that only cover generic drugs);
- When cost sharing for covered in-network services does not count toward the out-of-pocket limit;
- Limits on the number of visits or on specific dollar amounts payable under the health benefit plan; and
- When prior authorization is required for services.
The template and instructions indicate that qualified health plans (those certified and sold on the Marketplace) that cover excepted abortions (such as those in cases of rape or incest, or when a mother’s life is at stake) and plans that cover non-excepted abortion services must list “abortion” in the covered services box. Plans that exclude abortion must list it in the “excluded services” box, and plans that cover only excepted abortions must list in the “excluded services” box as “abortion (except in cases of rape, incest, or when the life of the mother is endangered).” Health plans that are not qualified health plans are not required to disclose abortion coverage, but they may do so if they wish.
By Danielle Capilla
Originally Posted By www.ubabenefits.com

by admin | May 1, 2017 | ACA, Benefit Management, Group Benefit Plans, Human Resources
 On April 18, 2017, the Department of Health and Human Services’ (HHS) Centers for Medicare & Medicaid Services (CMS) published its final rule regarding Patient Protection and Affordable Care Act (ACA) market stabilization.
On April 18, 2017, the Department of Health and Human Services’ (HHS) Centers for Medicare & Medicaid Services (CMS) published its final rule regarding Patient Protection and Affordable Care Act (ACA) market stabilization.
The rule amends standards relating to special enrollment periods, guaranteed availability, and the timing of the annual open enrollment period in the individual market for the 2018 plan year, standards related to network adequacy and essential community providers for qualified health plans, and the rules around actuarial value requirements.
The proposed changes primarily affect the individual market. However, to the extent that employers have fully insured plans, some of the proposed changes will affect those employers’ plans because the changes affect standards that apply to issuers.
The regulations are effective on June 17, 2017.
Among other things impacting group plans, the rule provided clarifications to the scope of the guaranteed availability policy regarding unpaid premiums. The guaranteed availability provisions require health insurance issuers offering non-grandfathered coverage in the individual or group market to offer coverage to and accept every individual and employer that applies for such coverage unless an exception applies. Individuals and employers must usually pay the first month’s premium to activate coverage.
CMS previously interpreted the guaranteed availability provisions so that a consumer would be allowed to purchase coverage under a different product without having to pay past due premiums. Further, if an individual tried to renew coverage in the same product with the same issuer, then the issuer could apply the enrollee’s upcoming premium payments to prior non-payments.
Under the final rule and as permitted by state law, an issuer may apply the initial premium payment to any past-due premium amounts owed to that issuer. If the issuer is part of a controlled group, the issuer may apply the initial premium payment to any past-due premium amounts owed to any other issuer that is a member of that controlled group, for coverage in the 12-month period preceding the effective date of the new coverage.
Practically speaking, when an individual or employer makes payment in the amount required to trigger coverage and the issuer lawfully credits all or part of that amount to past-due premiums, the issuer will determine that the consumer made insufficient initial payment for new coverage.
This policy applies both inside and outside of the Exchanges in the individual, small group, and large group markets, and during applicable open enrollment or special enrollment periods.
This policy does not permit a different issuer (other than one in the same controlled group as the issuer to which past-due premiums are owed) to condition new coverage on payment of past-due premiums or permit any issuer to condition new coverage on payment of past-due premiums by any individual other than the person contractually responsible for the payment of premiums.
Issuers adopting this premium payment policy, as well as any issuers that do not adopt the policy but are within an adopting issuer’s controlled group, must clearly describe the consequences of non-payment on future enrollment in all paper and electronic forms of their enrollment application materials and any notice that is provided regarding premium non-payment.
By Danielle Capilla, Originally Published By United Benefit Advisors

 The Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) requires employers to offer covered employees who lose their health benefits due to a qualifying event to continue group health benefits for a limited time at the employee’s own cost. Per regulation, qualifying events are specific events that cause or trigger an individual to lose health coverage. The type of qualifying event determines who the qualified beneficiaries are and the maximum length of time a plan must offer continuation coverage. A group health plan may provide longer periods of continuation coverage beyond the maximum 18 or 36 months required by law.
The Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) requires employers to offer covered employees who lose their health benefits due to a qualifying event to continue group health benefits for a limited time at the employee’s own cost. Per regulation, qualifying events are specific events that cause or trigger an individual to lose health coverage. The type of qualifying event determines who the qualified beneficiaries are and the maximum length of time a plan must offer continuation coverage. A group health plan may provide longer periods of continuation coverage beyond the maximum 18 or 36 months required by law.