by admin | Oct 30, 2025 | Custom Content, Employee Benefits, Health Care Costs
 No doubt about it, prescriptions are expensive. While this may not be a big worry when you’re young and healthy, the costs can add up quickly if you’re diagnosed with a chronic condition or need an expensive drug. Whether you take medications regularly or for an occasional illness, it pays to know how to save money on prescriptions.
No doubt about it, prescriptions are expensive. While this may not be a big worry when you’re young and healthy, the costs can add up quickly if you’re diagnosed with a chronic condition or need an expensive drug. Whether you take medications regularly or for an occasional illness, it pays to know how to save money on prescriptions.
Did You Know?
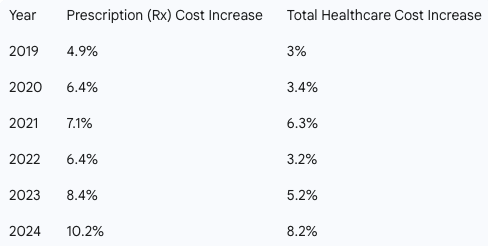
Drug costs are a primary driver of rising healthcare expenses for both employers and employees. Prescription drug spending is consistently growing at a faster rate than overall healthcare costs, with a steady increase of 6.8%. As the fastest-growing part of benefits plans, these costs will continue to climb with new pharmaceutical innovations.
For years in the U.S., cost has been a significant obstacle to sticking with medications with up to 3 in 10 people reporting that they do not take their medications as prescribed.
The Rising Cost of Prescriptions
Historically, prescription drug costs have outpaced total healthcare costs. The following chart highlights this trend from 2019 to 2024. 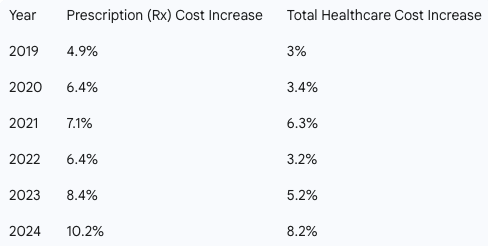
Prescription drug costs can put a strain on your budget, but with a little research and the right questions, you can reduce expenses without sacrificing your health.
Here are expert-backed strategies to help you save on your medications:
-
-
- Ask About a Generic Drug – Get the same quality and active ingredient as you’d find in a brand name, for less money.
- Save Money with a Pill Splitter – If your prescription comes in a higher dose that can be safely split, you get 2 doses for the price of 1.
- Consider a Combo Pill – Combining two drugs into one pill can help you avoid paying separate copays or coinsurance. Ask if a combo pill is an option for you.
- Buy in Bulk – Opt for a mail-order pharmacy to get a 90-day supply of your meds instead or a 30-day supply. This can often reduce your copay and overall cost.
- Make a List and Check it Twice – Check the list of preferred medications (a.k.a. “the formulary”), which tend to cost less.
- Find Out if You Still Need That Medication – If you’ve been taking the same medication for years, it’s worth checking in with your doctor to see if you still need it. Or if you’ve made a lifestyle change, it may reduce your need for certain medications. It never hurts to ask your doctor.
-
-
-
-
-
The medicines prescribed by your doctor are essential to your good health. With some savvy shopping, you can use the money you save on the things you enjoy!

by admin | Jul 6, 2018 | Benefit Management
Did you know that you can save time and money on your prescription drugs by simply signing up for a discount card online? With savings as much as 80% off, these discount cards keep your health care costs down even when the prices of prescriptions are sharply rising.


by admin | Jun 6, 2018 | Hot Topics, Human Resources
 Lately, there’s been a big focus on America’s opioid addiction in the news. Whether it’s news on the abuse of the drug or it’s information sharing on how the drug works, Americans are talking about this subject regularly. We want to help educate you on this hot topic.
Lately, there’s been a big focus on America’s opioid addiction in the news. Whether it’s news on the abuse of the drug or it’s information sharing on how the drug works, Americans are talking about this subject regularly. We want to help educate you on this hot topic.
Opioids are made from the opium poppy plant. Opium has been around since 3,400 BC and it was first referenced as being cultivated in Southwest Asia. The drug traveled the Silk Road from the Mediterranean to Asia to China. Since then, the drug has gained popularity for pain relief but it also has gained notoriety as an abused drug. Morphine, Codeine, and Heroin are all derived from the opium poppy and are all highly addictive drugs that are abused all around the world. As the demand for these drugs has increased, so has the production. From 2016 to 2017, the area under opium poppy cultivation in Afghanistan increased by 63 percent. In 2016, it killed some 64,000 Americans, more than double the number in 2005.
We can see that the danger from this drug is growing rapidly. What can we do to recognize potential abuse problems and to get help? Here are some facts about opioid addiction:
- How do they work? Opioids attach to pain receptors in your brain spinal cord, and other areas that recognize pain signals. As they attach to the receptors, it reduces the sending of pain messages to the brain and therefore reduces the feelings of pain in your body.
- Short-acting opiates are typically prescribed for injuries and only for a few days. They take 15-30 minutes for pain relief to begin and this relief lasts for 3-4 hours. Long-acting opiates are prescribed for moderate to severe pain and are used over a long period of time. Relief typically lasts for 8-12 hours and can be used alongside a short-acting drug for breakthrough pain.
- Dependence is common with long-term use of an opiate. This means that the patient needs to take more of and higher doses of the medicine to get the same pain relieving effect. This does not necessarily mean the patient is addicted. Addiction is the abuse of the drug by taking it in an unprescribed way—like crushing tablets or using intravenously.
- Help is available through many channels from private recovery centers to insurance providers. The Substance Abuse and Mental Health Services Administration helpline is 1-800-662-HELP. This line is confidential, free, and available 24-hours a day and 7 days a week. Family and friends may also call this number for resources for help. Additional resources can be found at drugabuse.com.
Make sure you are educated about the dangers of opioid abuse. But, don’t be discouraged and think that the abuse is incurable! There are many resources that can be used to break the addiction cycle and can make real change in the lives of its victims. Ask for help and offer help.

by admin | Jan 24, 2017 | Benefit Management, Employee Benefits
 Determining how an employer develops the most effective formulary, while protecting the financial stability of the plan, is certainly the challenge of this decade. Prescription management used to mean monitoring that the right people are taking medications to control their disease while creating strategies to move them from brand name to generic medications. With the dawn of specialty medications, formulary management has become a game of maximizing the pass-through of rebates, creating the best prior authorization strategies and tiering of benefits to create some barrier to more expensive medications, all without becoming too disruptive. As benefits managers know, that is a difficult challenge. The latest UBA Health Plan Survey revealed that 53.6 percent of plans offer four tiers or more, a 21.5 percent increase from last year and nearly a 55.5 percent increase in just two years. Thus, making “tiering” a top strategy to control drug costs. There are many additional opportunities to improve and help control the pharmacy investment, but focusing on the key components of formulary management and working on solutions that decrease the demands for medications are critical to successful plan management.
Determining how an employer develops the most effective formulary, while protecting the financial stability of the plan, is certainly the challenge of this decade. Prescription management used to mean monitoring that the right people are taking medications to control their disease while creating strategies to move them from brand name to generic medications. With the dawn of specialty medications, formulary management has become a game of maximizing the pass-through of rebates, creating the best prior authorization strategies and tiering of benefits to create some barrier to more expensive medications, all without becoming too disruptive. As benefits managers know, that is a difficult challenge. The latest UBA Health Plan Survey revealed that 53.6 percent of plans offer four tiers or more, a 21.5 percent increase from last year and nearly a 55.5 percent increase in just two years. Thus, making “tiering” a top strategy to control drug costs. There are many additional opportunities to improve and help control the pharmacy investment, but focusing on the key components of formulary management and working on solutions that decrease the demands for medications are critical to successful plan management.
When developing a formulary, Brenda Motheral, RPh, MBA, Ph.D., CEO of Archimedes, suggests that chasing rebates is not a strategy to optimize your investment. Some of the highest rebates may be from medications that add no better therapeutic value than an inexpensive medication that does not offer a rebate, but net cost is much lower than the brand or specialty medication being offered. Best formulary management will mean that specific medications that do not offer a significant therapeutic value are removed from the formulary, or are covered at a “referenced price” so the member pays the cost difference. Formulary management will need to focus on where the drug is filled and which medications are available.
When setting up parameters on where a drug is to be filled, the decision needs to be made if a plan will promote mail order. Mail order, if used and monitored appropriately, makes it more convenient for a patient to receive their regularly used medications and may provide savings. In fact, the UBA Health Plan Survey finds that more than one-third (36.3 percent) of prescription drug plans provide a 90-day supply at a cost of two times retail copays. But if mail order programs are not monitored, people can continue to receive medications that are no longer required and never used, adding to medical spend waste. Furthermore, in our analysis, we are finding that not all medications are less expensive through mail order, as shown in Figure 1 below. Therefore, examining the cost differential is critical in a decision to promote, or not promote, mail order.
Figure 1
| Drug Name |
Rx Category |
Mail Order |
Retail |
| Zytiga® |
Malignancies |
$8,749 |
$6,027 |
| Sumatriptan Succinate |
Migrane / Neurologic |
$575 |
$308 |
| Ranexa® |
Cardiovascular |
$259 |
$413 |
Another formulary consideration is in monitoring the increase in same drug pricing. The stories surrounding the price increases of EpiPens® has been well-documented, but how well do you understand the impact of price increases on your plan? Monitoring price increases, as shown in Figure 2, may help an employer turn to their pharmacy benefit manager (PBM) to ask for help in controlling these price increases, or help in decisions related to formulary inclusion.
Figure 2
| Drug Name |
Rx Category |
Plan Paid per
30-day Supply
(SPLY) |
Plan Paid per
30-day Supply |
| Cialis® |
Genito-Urinary / Acute Minor |
$287 |
$442 |
| AndroGel® |
Endocrine / Chronic Meidcal |
$471 |
$523 |
| Viagra® |
Genito-Urinary / Acute Minor |
$615 |
$978 |
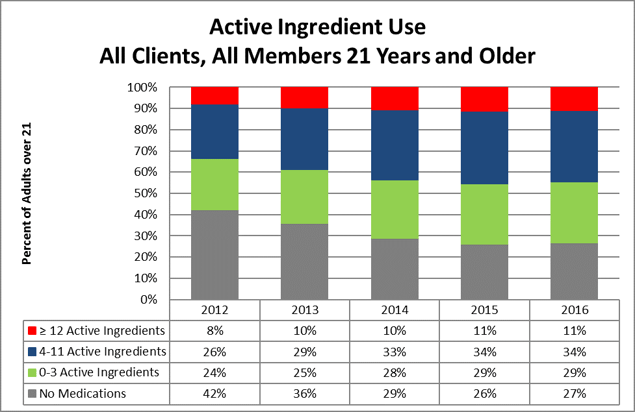
Formulary management solutions can become a cat-and-mouse game. The ultimate approach to manage the total spending on medications is by managing the growing demand. There has been significant press related to the opioid overutilization in the U.S., as illustrated in the article “Prescription Addiction.” But that issue is much broader in our society and relates to taking a pill as a quick solution to solve our medical problems. In March 2016, the Department of Health and Human Services (HHS) stated that 30 percent of the growth in spending related to medications was due to an increase in prescriptions per person. Certainly, medications should be used when there are no alternatives to control disease or pain. However, turning to medications as a first option for chronic condition control for issues like hypertension, blood sugar control, cholesterol control versus improving diet and exercise, etc., is just a band-aid solution that, in most cases, does not resolve the root issue. Yet, because this is sold as a quick fix, we see an increase in the number of individuals on medications. In 2012, 34 percent of plan members engaged in Vital Incite were taking four or more (active ingredients) medications, and that has grown to more than 45 percent in 2016. The data also illustrates that in 2012 more than 42 percent of members were not on any medications, but that group size has shrunk to only 27 percent. No formulary can impact this issue.
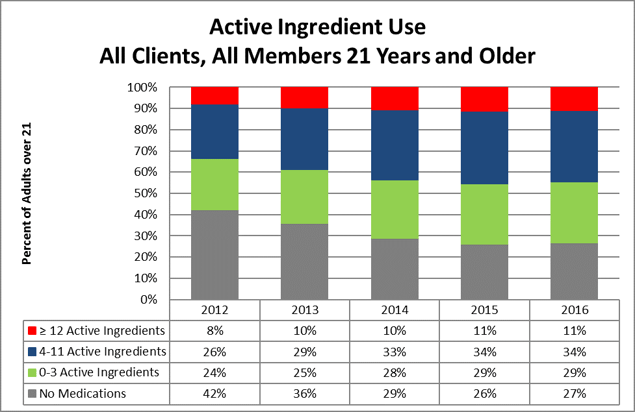
This increased use could be considered an improvement in care if their disease were more controlled. Appropriate and medically-impactful utilization would mean that a person is working toward improving diet and exercise and is taking the least expensive, yet effective, medication to control his or her disease.
Considering that diabetes medication options have really expanded, an employer would hope that the more expensive medication is providing the best control of disease. But, taking the medication alone will not control the disease and, at times, the progression of the medication cost can be related to progression of the disease due to a lack of disease management. For instance, a diabetic may have progressed from taking metphormin (marketed under the tradename Glucophage® among others), which costs approximately $27 per month, to metphormin ER (Glucophage® XR), which allows a person to take only one pill a day, so it may provide increased compliance, but costs $274 per month. Now, the option of taking Glumetza® is offered, which can be reimbursed at up to $3,620 per month, and is said to provide more stable results. But, if we examine the A1c control values from Vital Incite, do we find the reduction in A1c values as evidence that this additional investment in medication options is providing better control? Figure 3 provides an example of A1c control by prescription status. The goal would be that those on medications will become controlled. But, in our data, we are not seeing a significant improvement in persons with HgA1c levels above 7 percent. Control is achieved from diet, exercise, and appropriate medications. There are theories that people on these more expensive medications are using that as an approach to help them maintain their unhealthy behaviors. Therefore, taking medications alone does not appear to provide an effective solution and, in fact, providing chronic condition medications for free, without requiring any other effort, may not be the best investment for an employer.
Figure 3
| HgA1c Level |
In Treatment |
Untreated |
Discontinued
Treatment |
Possibly
Untreated |
| < 5.7 |
6 |
1 |
2 |
3 |
| 5.7 to 6.4 |
21 |
2 |
1 |
11 |
| 6.5 to 7.0 |
17 |
|
|
7 |
| > 7.0 |
53 |
4 |
|
5 |
In conclusion, determining which issues are having the most impact on an employer group will allow benefits managers to determine the company’s priorities. This is not an easy task, but with pharmacy spend increasing at a national average of 7.3 percent annually and becoming a higher percentage of the overall medical spend, new strategies need to be considered. Focusing on the key components that balance formulary management with the correct approach to manage the demand on medications can influence total pharmacy spend.
By Mary Delaney, United Benefit Advisors

 No doubt about it, prescriptions are expensive. While this may not be a big worry when you’re young and healthy, the costs can add up quickly if you’re diagnosed with a chronic condition or need an expensive drug. Whether you take medications regularly or for an occasional illness, it pays to know how to save money on prescriptions.
No doubt about it, prescriptions are expensive. While this may not be a big worry when you’re young and healthy, the costs can add up quickly if you’re diagnosed with a chronic condition or need an expensive drug. Whether you take medications regularly or for an occasional illness, it pays to know how to save money on prescriptions.