by admin | Dec 5, 2017 | Employee Benefits, Flexible Spending Accounts, IRS
 On November 2, 2017, House Republicans introduced a tax reform bill (H.R.1-115th Congress) called the “Tax Cuts and Jobs Act” that, if passed, would impact multiple aspects of the tax code. Many of these changes relate to employee benefit plans, particularly in relation to certain fringe benefits.
On November 2, 2017, House Republicans introduced a tax reform bill (H.R.1-115th Congress) called the “Tax Cuts and Jobs Act” that, if passed, would impact multiple aspects of the tax code. Many of these changes relate to employee benefit plans, particularly in relation to certain fringe benefits.
Dependent Care Accounts
A dependent care flexible spending account (DCFSA) is a pre-tax benefit account used to pay for eligible dependent care services. The IRS determines which expenses are eligible for reimbursement and these expenses are defined by Internal Revenue Code section 129 and the employer’s plan. Eligible DCFSA expenses include costs for adult day care centers, before and after school programs, child care, nannies, preschool, and summer day camp. Day nursing care, nursing home care, tuition for kindergarten and above, food expenses, and overnight camp are ineligible expenses. The employer determines the minimum election amount and the IRS determines the maximum election amount. The IRS sets the following annual contribution limits for a DCFSA:
- $2,500 per year for a married employee who files a separate tax return
- $5,000 per year for a married employee who files a joint tax return
- $5,000 per year for the head of household
- $5,000 per year for a single employee
The original version of the tax reform bill completely eliminated dependent care accounts. It is now reported that Representative Kevin Brady (R-Texas) has added an amendment to the bill that reverses the immediate repeal of DCFSAs, and would extend them for five more years.
Adoption Assistance
Employers may currently reimburse employees up to $13,570 (indexed) tax-free for qualified adoption expenses. This is eliminated in the bill.
Education Assistance
Employers may currently reimburse employees up to $5,250 on a tax-free basis for qualified education expenses. This is eliminated in the bill. Employers that are educational institutions can currently provide qualified tuition reductions to employees, their spouses, and dependents tax free, but this would be eliminated under the bill.
Employer Tax Deduction Impact
Under the proposed bill, employers’ corporate tax deduction credits for the following would be eliminated:
- Transportation fringe benefits
- On-premise athletic facilities
- Employer provided child care
The bill is now in markup, with the Ways and Means Committee working to draft a final bill for the House to vote on. If passed, it will be sent to the Senate to vote on.
By Danielle Capilla
Originally Published By United Benefit Advisors

by admin | Nov 14, 2017 | ACA, Group Benefit Plans, Human Resources, IRS
 October was a busy month in the employee benefits world. President Trump announced a new Acting Secretary for the U.S. Department of Health and Human Services (HHS). Eric Hargan fills the position vacated by Tom Price, who resigned in late September 2017. The U.S. Department of Labor (DOL) issued a proposed rule to delay a disability claims procedure regulation’s applicability date and HHS released its proposed rule on benefits and payment parameters for 2019. The U.S. Department of the Treasury (Treasury) issued its Priority Guidance Plan for projects it intends to complete during the first half of 2018.
October was a busy month in the employee benefits world. President Trump announced a new Acting Secretary for the U.S. Department of Health and Human Services (HHS). Eric Hargan fills the position vacated by Tom Price, who resigned in late September 2017. The U.S. Department of Labor (DOL) issued a proposed rule to delay a disability claims procedure regulation’s applicability date and HHS released its proposed rule on benefits and payment parameters for 2019. The U.S. Department of the Treasury (Treasury) issued its Priority Guidance Plan for projects it intends to complete during the first half of 2018.
DOL Proposes Delay to Final Disability Claims Procedures Regulations’ Applicability Date
The DOL issued a proposed rule to delay the applicability date of its final rule that amends the claims procedure requirements applicable to ERISA-covered employee benefit plans that provide disability benefits. The DOL’s Fact Sheet contains a summary of the final rule’s requirements.
The DOL is delaying the applicability date from January 1, 2018, to April 1, 2018, to consider whether to rescind, modify, or retain the regulations and to give the public an additional opportunity to submit comments and data concerning the final rule’s potential impact.
CMS Releases 2019 Benefits Payment and Parameters Proposed Rule
The Centers for Medicare & Medicaid Services (CMS) released a proposed rule and fact sheet for the 2019 Benefit Payment and Parameters. The proposed rule is intended to increase individual market flexibility, improve program integrity, and reduce regulatory burdens associated with the Patient Protection and Affordable Care Act (ACA) in many ways, including updates and annual provisions to:
- Essential health benefits
- Small Business Health Options Program (SHOP)
- Special enrollment periods (SEPs)
- Exemptions
- Termination effective dates
- Medical loss ratio (MLR)
CMS usually finalizes the Benefit Payment and Parameters rule in the first quarter of the year following the proposed rule’s release. November 27, 2017, is the due date for public comments on the proposed rule.
Almost all the topics addressed in the proposed rule would affect the individual market and the Exchanges, particularly the Small Business Health Options Program (SHOP) Exchanges.
Of interest to small group health plans, CMS proposes to change how states will select essential health benefits benchmark plans. If CMS keeps this change in its final rule, then it will affect non-grandfathered small group health plans for benefit years 2019 and beyond.
Treasury Issues its Priority Guidance Plan
The Treasury issued its 2017-2018 Priority Guidance Plan that lists projects that it intends to complete by June 30, 2018, including:
- Guidance on issues related to the employer shared responsibility provisions
- Regulations regarding the excise tax on high cost employer-provided coverage (“Cadillac tax”)
- Guidance on Qualified Small Employer Health Reimbursement Arrangements (QSE HRAs)
By Danielle Capilla
Originally Published By United Benefit Advisors

by admin | Nov 9, 2017 | ACA, Human Resources, IRS

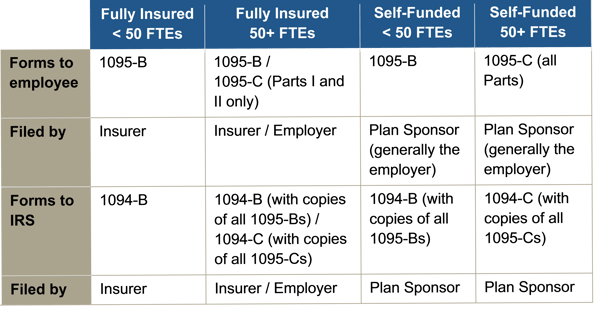
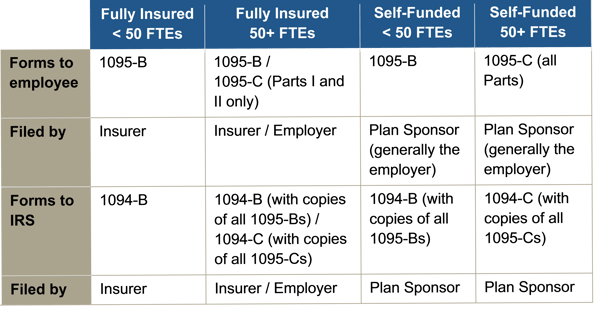
Instructions for both the 1094-B and 1095-B and the 1094-C and 1095-C were released, as were the forms for 1094-B, 1095-B, 1094-C, and 1095-C.
Reporting will be due early in 2018, based on coverage in 2017. For calendar year 2017, Forms 1094-C, 1095-C, 1094-B, and 1095-B must be filed by February 28, 2018, or April 2, 2018, if filing electronically. Statements to employees must be furnished by January 31, 2018. In late 2016, a filing deadline was provided for forms due in early 2017, however it is unknown if that extension will be provided for forms due in early 2018. Until employers are told otherwise, they should plan on meeting the current deadlines.
All reporting will be for the 2017 calendar year, even for non-calendar year plans.
The reporting requirements are in Sections 6055 and 6056 of the ACA. The major reporting requirements are:

by admin | Oct 26, 2017 | Benefit Management, Benefit Plan Tips, Tricks and Traps, Human Resources

Fall. With it comes cooler temperatures’, falling leaves, warm seasonal scents like turkey and pumpkin pie, and Open Enrollment. It goes without saying; employees who understand the effectiveness of their benefits are much more pleased with those packages, happier with their employers, and more engaged in their work. So, as your company gears up for a new year of navigating Open Enrollment, here are a few points to keep in mind to make the process smoother for both employees and your benefits department. Bonus: it will lighten the load for both parties alike during an already stress-induced season.
Communicate Open Enrollment Using a Variety of Mediums
Advertise 2018 benefit changes to employees by using a variety of mediums. The more reminders and explanation of benefits staff members have using more than one mode of media, the more likely employees will go into Open Enrollment with more knowledge of your company’s benefit options and when they need to have these options completed for the new year.
- Consider explainer videos to simplify the amount of emails and paperwork individuals need to review come Open Enrollment time. These videos can increase the bottom line as well, eliminating the high cost of print material.
- Opt for placards placed throughout your high-traffic areas. Communicate benefit options and remind employees of Open Enrollment dates for the new year by posting in such areas as the lobby, break room and bathroom stalls.
- Choose SMS texting. Today, over 97% of individuals use text. Ninety-eight percent of those that use text open messages within the first three minutes of receiving them; 6-8 times higher than the engagement rate for email. Delivering a concise message to employees’ mobile devices creates more touch points along the Open Enrollment journey. The key, however, is making it quick so as to entice your employees to take action.
- Promote apps and in-app tools. Push notifications and apps like Remind 101 can help drive employee engagement during Open Enrollment season simply by providing short messages reminding them to enroll. Notifications like these can also be tailored to unique employee groups based on location, job level, eligibility status and more.
Utilize Mobile Apps and Web Portals for Open Enrollment
Now that your company has communication down pat for Open Enrollment, simplify the arduous task employees have of enrolling for the coming year by going paperless. Utilize web portals through benefit brokers and companies like ADP to eliminate the hassle of employees having to fill out paperwork both at renewal, and at the time of hire. With nearly three quarters of individuals in the United States checking their phone once an hour and 90% percent of this time is spent using one app or another as a main source of communication, mobile apps can make benefits engagement much easier due to the anywhere/anytime accessibility they offer.
The personal perks for employees are great too! Staff members with a major lifestyle event can make benefit adjustments quickly with the ease of mobile apps. Employees recognize this valuable and time-saving trend and enjoy having this information at their fingertips.
Open Enrollment season can be a stressful time but hopefully these tips will help for a smoother transition into the next year for your business. Simple things like using explainer videos, placing reminders in high traffic areas and utilizing mobile apps and text messaging can save time and stress in the long run for your employees and benefit department.

by admin | Oct 16, 2017 | Health & Wellness, Hot Topics, Human Resources
 There are places where you expect things to be noisy, such as a rock concert, and places where you expect it to be quiet, like an office. And while nobody likes being “shushed,” there are few things more annoying than trying to work when someone else is talking in the background.
There are places where you expect things to be noisy, such as a rock concert, and places where you expect it to be quiet, like an office. And while nobody likes being “shushed,” there are few things more annoying than trying to work when someone else is talking in the background.
The ‘80s music group ‘Til Tuesday said it best: “Hush hush, keep it down now, voices carry.” An article in Human Resource Executive Online titled, “A Not-So-Quiet Little Problem: Noise!,” points out the current problem of modern, open offices—NOISE. When offices had doors, or at least cubicles, along with sound-absorbing carpeting and ceiling tiles, background noise wasn’t such a problem. Now, however, offices are wide open with nothing to block sound waves. Combine that with hardwood, or concrete floors, lots of glass and tall, echoing ceilings, and you’ve got the perfect storm for noise pollution.
Forward-thinking, or technology companies especially like open offices, and you can imagine what it sounds like with people talking on the phone, banging away at their keyboards, and conversing with each other. According to the article, nobody considers the acoustics of a room. They look at how beautiful, modern, and spacious it is. Then, once the room is filled with busy employees, the shock of its lack of tranquility sets in.
Employees become distracted by the noise, which in turn leads to reduced productivity. You can tell a lot about the noise level of an office by how many employees are wearing headphones. For workers to feel “healthy” at work, noise is a major factor, along with air quality and temperature.
There are many ways to fix a noisy office if you follow the A, B, Cs—absorb, block, cover. Materials can be placed to absorb noise, walls or furniture can be positioned to block noise, and there are electronic devices that use counter-measures to cover noise. The industry, office layout, and other factors will influence the choice of the best solution to mitigate noise. One thing is certain: when choosing a new office, or remodeling an existing one, it’s best to factor in a room’s acoustics along with its aesthetics.
By Geoff Mukhtar
Originally posted by www.UBABenefits.com

 On November 2, 2017, House Republicans introduced a tax reform bill (H.R.1-115th Congress) called the “Tax Cuts and Jobs Act” that, if passed, would impact multiple aspects of the tax code. Many of these changes relate to employee benefit plans, particularly in relation to certain fringe benefits.
On November 2, 2017, House Republicans introduced a tax reform bill (H.R.1-115th Congress) called the “Tax Cuts and Jobs Act” that, if passed, would impact multiple aspects of the tax code. Many of these changes relate to employee benefit plans, particularly in relation to certain fringe benefits.