by admin | Apr 3, 2024 | Employee Benefits
 Free and low-cost employee benefits are perks that don’t cost you much financially. These perks are often simple to provide and help enhance an existing employee benefits package. Including non-traditional benefits in a job offer shows employees your values; they’re a promise to both current and potential employees that you’ll support them and treat them right.
In the competitive race for talent, employers might consider providing the following affordable employee perks to appeal to workers:
Free and low-cost employee benefits are perks that don’t cost you much financially. These perks are often simple to provide and help enhance an existing employee benefits package. Including non-traditional benefits in a job offer shows employees your values; they’re a promise to both current and potential employees that you’ll support them and treat them right.
In the competitive race for talent, employers might consider providing the following affordable employee perks to appeal to workers:
- Health Savings Accounts (HSAs) or Flexible Savings Accounts (FSAs) – Even if an organization cannot provide comprehensive healthcare benefits, providing FSAs or HSAs enables employees to allocate pre-tax funds for medical expenses, easing their financial load.
- Prioritizing Work/Life Balance – With remote work now more common as a result of the pandemic, most employees expect and appreciate greater flexibility in the workplace. In fact, 67% of people think having work/life balance is more important than their pay and employee benefits combined. Hybrid work, Paid Time Off (PTO), and flexible work hours allow employees to juggle other responsibilities, such as caring for young children or aging parents.
- Learning and Professional-Development Opportunities – Establishing a culture that supports continuous learning can help foster a mindset of growth and professional development among your workforce. Investing in professional growth opportunities, such as conferences, workshops, online courses or mentorships, demonstrates a commitment to their long-term success.”
- Mental Health Perks – Mental health is just as important as physical health and more and more employers are prioritizing it. Offering an Employee Assistance Program (EAP) that includes therapy sessions and support, mindfulness apps, and mental health days are a few ideas to encourage strong mental health.
- Paid Volunteer Time – Encouraging community engagement is possible for employers through the provision of paid time off, allowing employees to volunteer with charitable organizations. Giving back to the community not only instills a sense of purpose and fulfillment but also can strengthen team bonds.
- Employee Recognition Programs – An “emotional salary” contributes to an employee’s sense of being adequately rewarded at work, playing a significant role in job satisfaction. When employees experience a sense of value, recognition, and appreciation for their contributions, they are more likely to enjoy their work and find it meaningful. Employers can implement a system to publicly acknowledge and reward employees for their work.
- Financial Education Workshops – More employees today want guidance to increase their financial literacy. To address this demand, employers can offer resources or workshops focusing on personal finance management, budgeting, and retirement planning. Empowering employees with financial literacy can enhance overall well-being and relieve stress.
- Summer Hours and/or Casual Dress Code – Allowing casual dress on certain days allows workers to be themselves which contributes to a sense of belonging in the workplace. This could include casual Fridays or a relaxed dress code during the hot summer months. Additionally, closing an hour or two early on a Friday demonstrates flexibility and can improve employees’ work/life balance during vacation season.
You don’t need to have a fat wallet or offer more employee benefits than your competitors to win over top talent. These low or no-cost perks that employees value create a fulfilling work environment that, in turn, attracts and retains top talent!

by admin | Feb 2, 2024 | Employee Benefits
 The challenges that influenced the benefits landscape in 2023 persist—perhaps even more so. Rising costs, due to inflation and increasing health care prices, will continue to present challenges this new year. But employers who understand the benefits landscape for 2024 can mold their approach for the upcoming year.
The challenges that influenced the benefits landscape in 2023 persist—perhaps even more so. Rising costs, due to inflation and increasing health care prices, will continue to present challenges this new year. But employers who understand the benefits landscape for 2024 can mold their approach for the upcoming year.
A new year means revisiting your existing benefits strategy and looking at the top benefit trends:
Financial Wellness Benefits
Employees worry and stress about their finances and are searching for financial wellness education and guidance. Nearly 80% of employees say a financial wellness benefit is an important part of a comprehensive benefits package. Some of the popular financial wellness benefits are:
- Retirement Plan Options with Matching Contributions
- Health Savings Accounts
- Flexible Spending Accounts
- Financial Planning Assistance
- Flexible Paydays
- Employee Discount Program
- Financial Reimbursements (Ie. student loan repayment plans, child-care support funds and professional development stipends)
Voluntary Benefits
You can please some of the people some of the time, but you can’t please all the people all the time – unless you embrace voluntary benefits, that is. Voluntary benefits are optional perks that are offered to employees at a discounted group rate which their employer has negotiated with providers. While employees still need to pay to use these benefits, the amount is usually far less than it would be without company subsidies.
Moving forward, we can expect to see more sophisticated customization tools that allow employees to choose the benefits that best align with their individual circumstances and priorities. Whether it’s affordable veterinary insurance for pet owners, subsidized pre-K childcare for parents, or student loan repayment programs, offering these types of policies can directly improve the quality of life for employees who choose to take advantage of them.
Enhanced Family Benefits
Employers are increasingly looking to expand their family-friendly benefits for employees to better support employees in their caregiving roles.
- Paid family leave is not guaranteed by law in the U.S. but it is a highly sought-after perk. A parental leave policy – one that considers both parents and accounts for adoption and fostering in addition to childbirth – can show your employees you care about supporting their home lives.
- Childcare assistance supports working parents facing rising costs of living. While some larger employers may offer on-site childcare, smaller businesses can show their commitment to working parents by helping to subsidize the cost of childcare through employer contributions or pre-tax deductions.
- Fertility assistance supports employees who are going through costly infertility treatments, surrogacy, and IVF.
With four generations represented in the workforce, the support offered by employers can look different to Baby Boomers caring for their parents than a Millennial or Gen Zer caring for their children.
Inclusive and Flexible Care
The diverse workforce of 2024 is prioritizing a better work-life balance. It’s important to develop a benefits package that recognizes a healthy environment for your employees.
- Mental health benefits are in demand since mental health is a crucial part of overall health. Offering an employee assistance program (EAP) is a great way to support workers in tough situations.
- Work flexibility includes not only remote or hybrid work options, but you can also consider flexible start and stop times, a four-day work week or unlimited PTO to attract top talent and increase retention.
Overall, your benefits offerings for 2024 should reflect your organization’s values. Remember, your company depends on being able to keep your employees happy, healthy, and productive. Benefits that show respect for employees and promote a strong, vibrant culture are worth the investment.

by admin | Jan 8, 2024 | Employee Benefits
 For most organizations, employee benefits communication kicks into high gear during open enrollment season. During this time, there is a surge in emails, educational webinars, fliers throughout the office, and a barrage of forms demanding signatures.
For most organizations, employee benefits communication kicks into high gear during open enrollment season. During this time, there is a surge in emails, educational webinars, fliers throughout the office, and a barrage of forms demanding signatures.
Post open enrollment, however, employees often receive minimal information about their benefits. While sporadic email updates or new laminated signs in the office kitchen may occur, a comprehensive, year-round employee benefits communication plan is often lacking.
This oversight represents a significant missed opportunity. An annual approach is insufficient to ensure that employees genuinely comprehend and effectively utilize their benefits.
When employers use a year-round approach to fully educate their employees on their benefits offerings, employees benefit both in their personal well-being and financial security. Employers also benefit from increased employee engagement, leading to a more creative work environment, reduced stress levels, higher employee retention rates, and potentially higher profitability. Establishing a year-round employee benefits communication plan is crucial.
One way to establish an engaging year-round employee communication plan is through a calendar-based approach. Creating a monthly or quarterly calendar allows for the concentration on a series of topics related to benefits throughout the year. Q4 is the optimal period to highlight open enrollment, while the remaining three quarters provide an opportunity to dive into specific benefit categories such as health, lifestyle, and wealth.
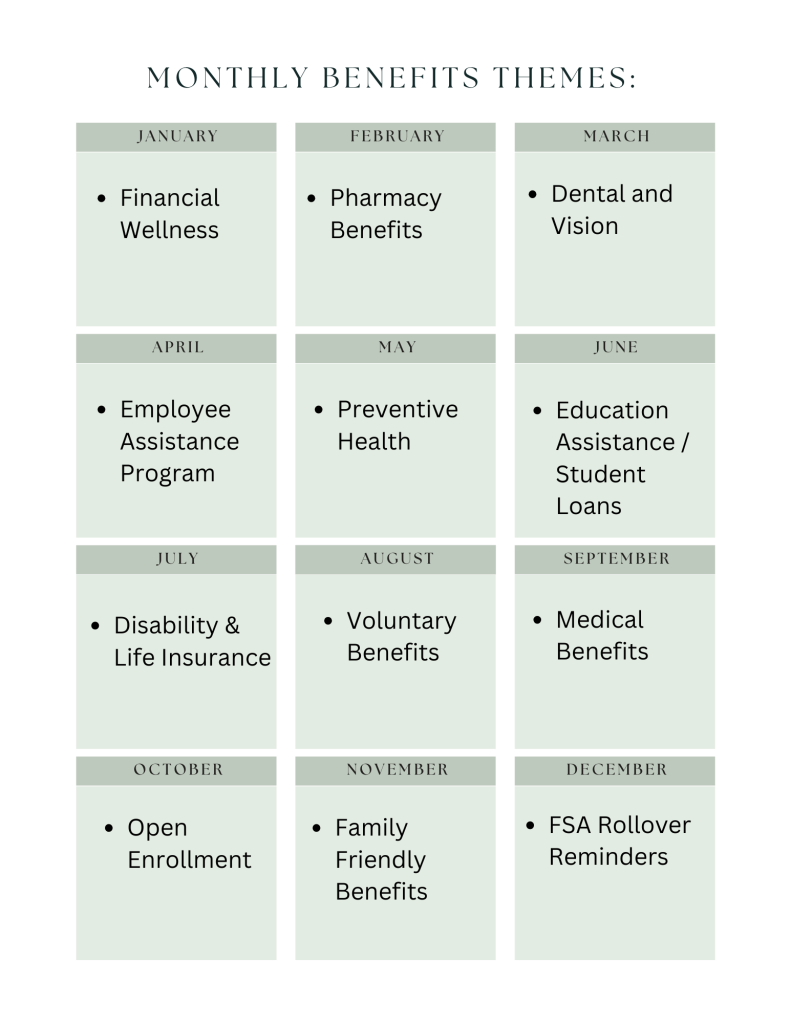
Think about what will be on the top of employee’s minds over the next several months and create a calendar that speaks to those needs. Here is an example of a quarterly calendar:
Q1: In the beginning of the new year, the mantra is “New Year, New You!” What benefits can help employees plan for their future throughout the year – and take the stress out of the decision-making process?
Q2: With the weather beginning to warm up and the beginning of spring, many employees start to be more active and spend more time outdoors. What benefits address overall health and well-being?
Q3: Summertime means vacations for many families. This is a good time to address a healthy work-life balance and to give reminders about time off and childcare benefits.
Q4: When the weather starts to turn cooler, Q4 is in full gear! And that means one thing: Open Enrollment Season. Do your employees have the information to help them pick the right plan for the upcoming year?
Here is an example of some themes to incorporate into a monthly calendar:
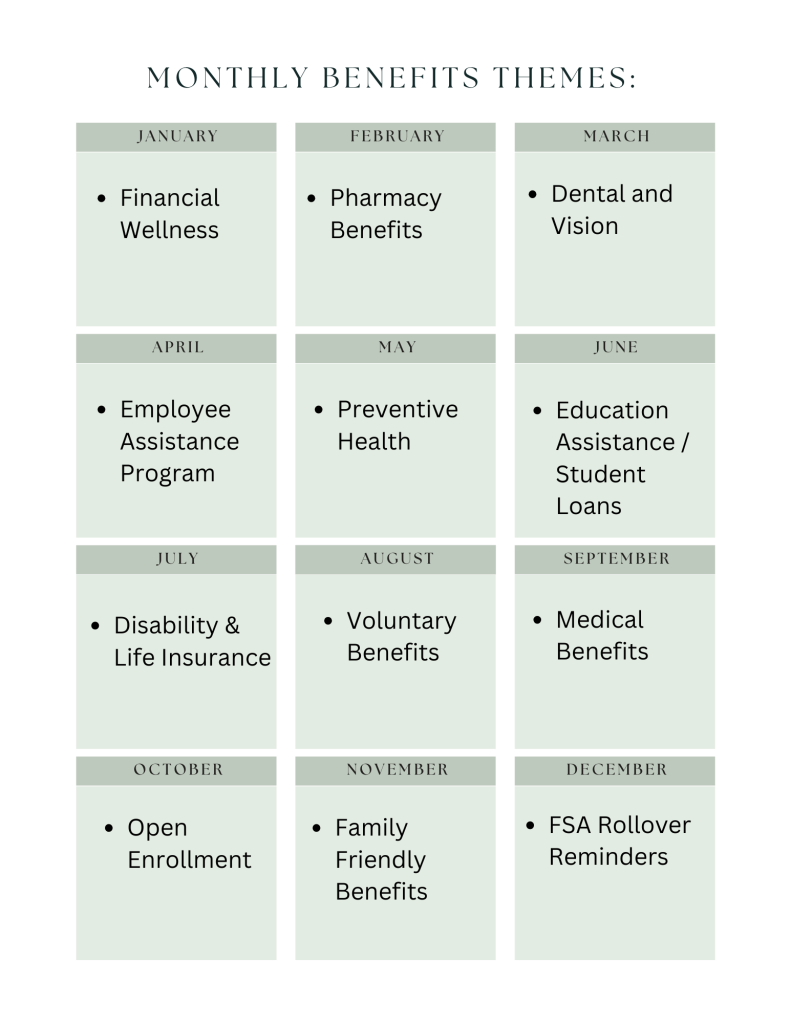
Benefits education is communicating information about available benefits in ways that employees can connect to and understand. Communicating benefits information year-round is important because employees’ lives – and their situations – are constantly changing. They get married, divorced, adopt a child or have medical challenges arise. They are thinking about their health and financial security and how to adapt to it. If employees are engaged with their benefits throughout the year, they are more likely to value and use their benefits and will be better informed about their decisions and/or changes they need to make during the next Open Enrollment period!

by admin | Nov 29, 2023 | Employee Benefits, Health Insurance
 If you have a health plan through a job, you can use a Flexible Spending Account (FSA) to pay for health care costs, like deductibles, copayments, coinsurance, and some drugs. They can lower your taxes.
If you have a health plan through a job, you can use a Flexible Spending Account (FSA) to pay for health care costs, like deductibles, copayments, coinsurance, and some drugs. They can lower your taxes.
How Flexible Spending Accounts work
A Flexible Spending Account (FSA, also called a “flexible spending arrangement”) is a special account you put money into that you use to pay for certain out-of-pocket health care costs.
You don’t pay taxes on this money. This means you’ll save an amount equal to the taxes you would have paid on the money you set aside.
Employers may make contributions to your FSA, but they aren’t required to.
With an FSA, you submit a claim to the FSA (through your employer) with proof of the medical expense and a statement that it hasn’t been covered by your plan. Then, you’ll get reimbursed for your costs. Ask your employer about how to use your specific FSA.
To learn more about FSAs:
Facts about Flexible Spending Accounts (FSA)
- They are limited to $3,050 per year per employer. If you’re married, your spouse can put up to $3,050 in an FSA with their employer too.
- You can use funds in your FSA to pay for certain medical and dental expenses for you, your spouse if you’re married, and your dependents.
- You can spend FSA funds to pay deductibles and copayments, but not for insurance premiums.
- You can spend FSA funds on prescription medications, as well as over-the-counter medicines with a doctor’s prescription. Reimbursements for insulin are allowed without a prescription.
- FSAs may also be used to cover costs of medical equipment like crutches, supplies like bandages, and diagnostic devices like blood sugar test kits.
- Get a list of generally permitted medical and dental expenses from the IRS.
- You can’t use a Flexible Spending Account with a Marketplace plan.
FSA limits, grace periods, and carry-overs
You generally must use the money in an FSA within the plan year. But your employer may offer one of 2 options:
- It can provide a “grace period” of up to 2 ½ extra months to use the money in your FSA.
- It can allow you to carry over up to $610 per year to use in the following year.
Your employer doesn’t have to offer these options. If it does, it can be either one of these options, but not both.
Plan ahead At the end of the year or grace period, you lose any money left over in your FSA. Don’t put more money in your FSA than you think you’ll spend within a year on things like copayments, coinsurance, drugs, and other allowed health care costs.
Originally posted on Healthcare.gov

by admin | Nov 2, 2023 | Employee Benefits
 The connection between employee wellness and the benefits of the job might seem obvious. But the conversation should be more nuanced than merely a discussion about health insurance, access to mental healthcare like employee assistance programs (EAPs), and well-being apps to reach zen.
The connection between employee wellness and the benefits of the job might seem obvious. But the conversation should be more nuanced than merely a discussion about health insurance, access to mental healthcare like employee assistance programs (EAPs), and well-being apps to reach zen.
Indeed, Human Resources professionals must reconsider their definition of benefits. It must extend to all the pros of working at a company. This includes the compensation and benefits packages but also other benefits like the team vibe, how managers treat employees, the expectations of employees, the ability for work-life balance, etc.
The New Human Resources
Thinking about this link between wellness and benefits is a key differentiator between traditional approaches to HR and the transformational employee-centric approach of the here and now. In the wake of the pandemic and the arrival of Gen Z employees to the workforce, expectations of employment have changed. HR must put emphasis on empathetic leadership, collegiality, and support for the health and wellness of the team for both recruiting and retention purposes.
HR’s Desire to Support Employee Wellness
The will to support employee mental health and wellness is there. Dating back to the State of HR 2022, when HR leaders who responded to the HR Exchange Network survey made employee engagement the top priority, organizations have been clamoring to improve recruiting, engagement, and retention. The foundation for this crusade is focusing on employee wellness. After all, at the heart of these efforts is job satisfaction.
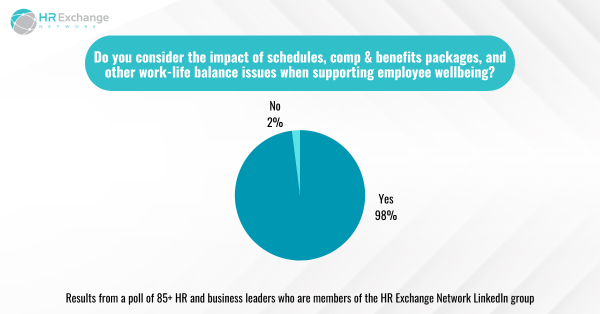
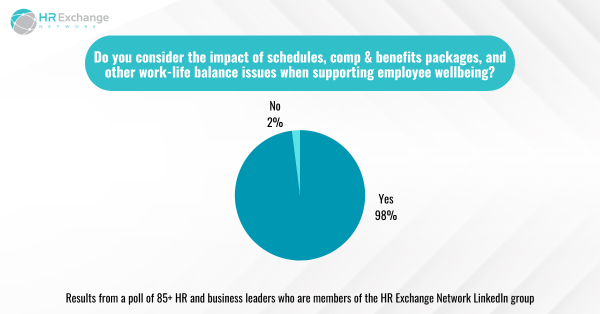
Many HR professionals have great intentions when considering a broader definition of benefits of a job. A whopping 98% of respondents to an HR Exchange Network LinkedIn poll say they consider the impact of schedules, compensation and benefits packages, and other work-life balance issues when supporting employee wellbeing.
Is HR Living Up to Its Ambition?
While most in HR say they want to help employees manage their mental health and wellness, they know employees might not have realized their efforts yet.
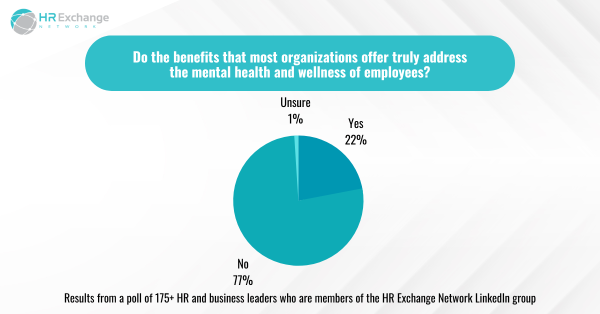
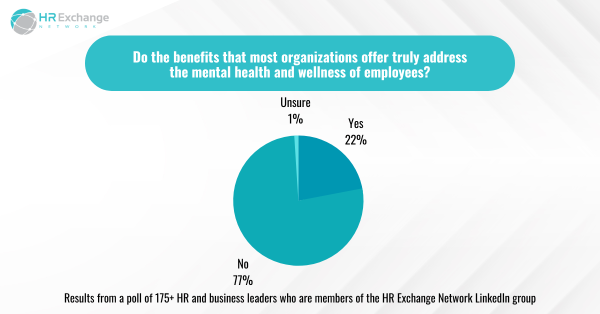
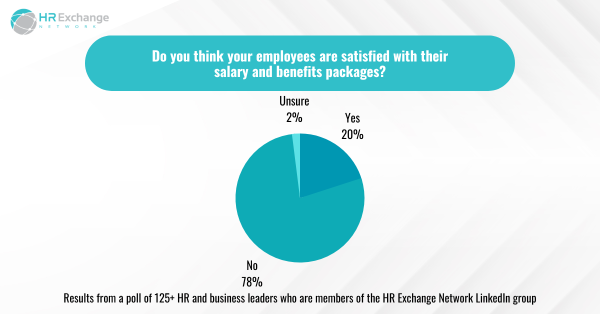
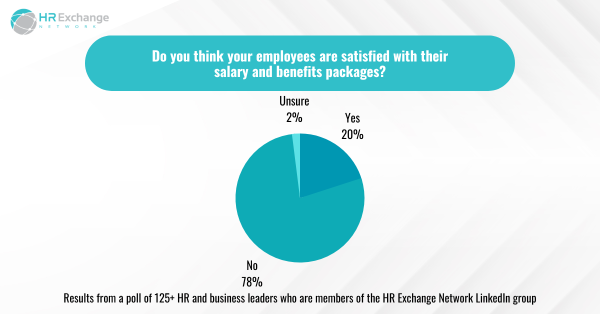
More than 75% – an overwhelming majority – of respondents to another HR Exchange Network LinkedIn poll said that the benefits most organizations offer do not truly address the mental health and wellness of employees. In addition, 78% in another poll on LinkedIn said employees were not satisfied with their salary and benefits packages.
Clearly, most in HR have more work to do when it comes to wellness and benefits. The first step would be to evaluate the company’s offerings. In 2022, respondents to the State of HR said the following were the top five benefits to offer or under consideration:
- Medical, dental, or vision insurance (55%)
- Wellness programs (53%)
- EAPs (45%)
- Mental health coaching (38%)
- Retirement savings (33%)
Worth noting, in the 2023 survey, 20% said they planned to invest in EAPs. In addition, the respondents of that survey shared their top priorities for addressing mental health and wellness:
- Creating a supportive environment for employees to talk about mental health concerns (40%)
- Implementing policies and procedures that address mental health in the workplace (37%)
- Providing accommodations for employees with mental health conditions (34%)
- Encouraging employees to take time off or seek medical attention (33%)
- Gyms/partnerships/fitness apps/fitness classes (27%)
Next Steps
Transformation requires effort and can be slow. Human Resources realizes that employees expect employers to support their mental health and wellness. Until now, that expectation – if ever met – was simply about offering the right kind of insurance and access to mental healthcare. Now, leaders and managers are meant to be empathetic and able to recognize those in need of help. Frankly, most have not had any sort of training, and it’s probably unfair to expect this of them. HR professionals are honest about the lack of support managers are receiving:

Presumably, the next step is to better train managers to provide mental health and wellness support and ensure the business builds itself around a people-centric culture. Certainly, the top priorities of HR professionals in 2023 suggest that employees are gaining leverage with HR:
- Developing and implementing diversity, equity, and inclusion (DEI) initiatives (22%)
- Improving employee engagement and retention (21%)
- Recruiting and retaining top talent (15%)
In fact, DEI is directly related to wellness at work because those efforts contribute to people feeling as though they are treated fairly and included. Providing that sense of belonging is an essential part of wellness, as is improving engagement and retention. To recruit and keep top talent, employers must continue to care for employees and lead HR with heart.
By Francesca Di Meglio
Orignally Posted on HR Exchange Network

by admin | Oct 25, 2023 | Employee Benefits, Health Insurance
 Not understanding benefits terminology is near the top of the list of ways that open enrollment and benefits selection can stress you out. Open enrollment is coming quickly and soon you will be talking about benefit options. The world of benefits and insurance can be confusing. In-network, out-of-network, deductibles, co-pays and co-insurance? What?
Not understanding benefits terminology is near the top of the list of ways that open enrollment and benefits selection can stress you out. Open enrollment is coming quickly and soon you will be talking about benefit options. The world of benefits and insurance can be confusing. In-network, out-of-network, deductibles, co-pays and co-insurance? What?
Let us help break it down:
Premium – a monthly payment you make to your health insurance provider- it is the cost of having health insurance coverage. It’s perhaps the easiest component of a health plan – it’s the equivalent of a sticker price.
Here’s how it works: Coverage itself varies considerably from one health plan to another but in general, the less you pay for your coverage, the more you’re likely to have to pay when you need health care – and vice versa.
Co-insurance – A percentage of a health care cost—such as 20 percent—that the covered employee pays after meeting the deductible.
How it works: Let’s say you’ve paid $1,500 in health care costs and met your deductible. When you go to the doctor, instead of paying all costs, you and your plan share the cost. For example, your plan may pay 80% so then your share would be the remaining 20%.
Co-payment – The fixed dollar amount—such as $25 for each doctor visit—that the covered employee pays for medical services or prescriptions.
How it works: After your co-pay, your insurance picks up the rest of the bill for that visit. Co-pays typically count toward your annual out-of-pocket maximum (but there can be exceptions depending on your plan). The amount can vary depending on where you go for care, the type of doctor you see, and the type of prescription you are taking.
Deductible – How much you pay before your health insurance coverage kicks in. Your deductible resets every year.
How it works: If your plan’s deductible is $1,500, you’ll pay 100% of health care expenses until the bills total $1,500. After that, you share the cost with your plan by paying co-insurance.
Network – “In-network” refers to doctors and other health providers that are part of the insurer’s preferred network. Insurers sign contracts and negotiate prices with these in-network providers. This isn’t the case for “out-of-network” providers.
Here’s why that matters: Expenses you incur for services provided by out-of-network professionals may not be covered or may only be partially covered by your insurance; you will generally have a higher deductible and out-of-pocket limit when you see an out-of-network provider.
Out-of-pocket Maximum (OOPM) – the absolute most you pay in one year for your health care expenses before your insurance covers 100% of the bill.
Here’s how it works: What you pay toward your plan’s deductible, co-insurance and co-pays are all applied to your out-of-pocket max. If your plan covers more than one person, you will likely have a family out-of-pocket max and an individual out-of-pocket max. That means:
- When the deductible, co-insurance and co-pays for one person reach the individual maximum, your plan then pays 100% of the expenses for that person.
- When what you’ve paid toward individual maximums adds up to your family’s out-of-pocket max, your plan will pay 100% of the expenses for everyone on the plan.
Picking health insurance can be a dizzying adventure and making a mistake can be costly since you are generally locked into your health insurance for one year, with very limited exceptions. But when you understand how open enrollment works and how it impacts your family’s household budget, you can make wise, informed choices.

 Free and low-cost employee benefits are perks that don’t cost you much financially. These perks are often simple to provide and help enhance an existing employee benefits package. Including non-traditional benefits in a job offer shows employees your values; they’re a promise to both current and potential employees that you’ll support them and treat them right.
In the competitive race for talent, employers might consider providing the following affordable employee perks to appeal to workers:
Free and low-cost employee benefits are perks that don’t cost you much financially. These perks are often simple to provide and help enhance an existing employee benefits package. Including non-traditional benefits in a job offer shows employees your values; they’re a promise to both current and potential employees that you’ll support them and treat them right.
In the competitive race for talent, employers might consider providing the following affordable employee perks to appeal to workers: